As we approach another Medicare ACO performance year, now in the REACH model as opposed to Direct Contracting, we’ve refreshed our FAQ article from last year that breaks down the Primary Care Capitation (PCC) concept into an easy to understand format. We encourage all new and returning Participating PCPs to read this blog post to ensure they’re ready to hit the ground running in 2023.
For many primary care providers (PCPs) and their practices, entering the world of value-based care can be overwhelming and complicated. Managing traditional Medicare fee-for-service (FFS) patients under a CMS-calculated budget is value-based care in its simplest form. The Direct Contracting (DC) model builds upon this structure and introduces a new concept developed to avoid the volatility of FFS and provide PCPs with increased revenue stability and more predictable cash flow for their aligned Medicare patients: Base Primary Care Capitation (BPCC).
If you’re a PCP joining a Direct Contracting Entity (DCE) in 2022, there is still a lot to comprehend about how capitation will impact your monthly revenue in advance of the January 1st start date. In this article, we will address providers’ most Frequently Asked Questions regarding BPCC with the goal of empowering PCPs to take advantage of capitation in the new CMS DC model.
Note: Capitation is the remittance to providers of a fixed reimbursement that is not tied to the volume of healthcare services provided. In other words, rather than receiving compensation for each patient visit or procedure, providers get a set reimbursement based on their assigned population. We previously published an overview of the various forms of capitation in Direct Contracting if you need a quick refresher on some of the fundamentals.
BPCC is a monthly payment from CMS to the DC Entity meant to represent the cost of providing primary care services to their aligned DC beneficiaries. The DCE then determines how much BPCC is allotted to each participating provider based on the number of beneficiaries aligned to the PCP, and distributes monthly payments accordingly. This capitated amount replaces providers’ fee-for-service primary care revenue (for aligned DC beneficiaries only).
Note: While participating PCPs do not need to convert 100% of their revenue from FFS to capitation, all providers Pearl assists in the DC model are fully capitated. However, should a provider participate in a DCE and choose to take only a 50% FFS reduction (as an example), they would get half of the calculated BPCC and receive 50% of Medicare’s listed rates for any FFS claims they submit to CMS.
BPCC is calculated by looking at the proportion of the total cost of care (TCoC) that is attributed to the primary care services that a PCP provided to their Medicare FFS patients over a specific period of time (e.g., for performance year 2022, it is based on the first three quarters of 2021). This proportion is then applied to the anticipated TCoC for the provider’s beneficiaries, i.e., the benchmark. The result is a per-beneficiary-per-month (PBPM) amount for each beneficiary aligned to the DCE’s participating PCPs.
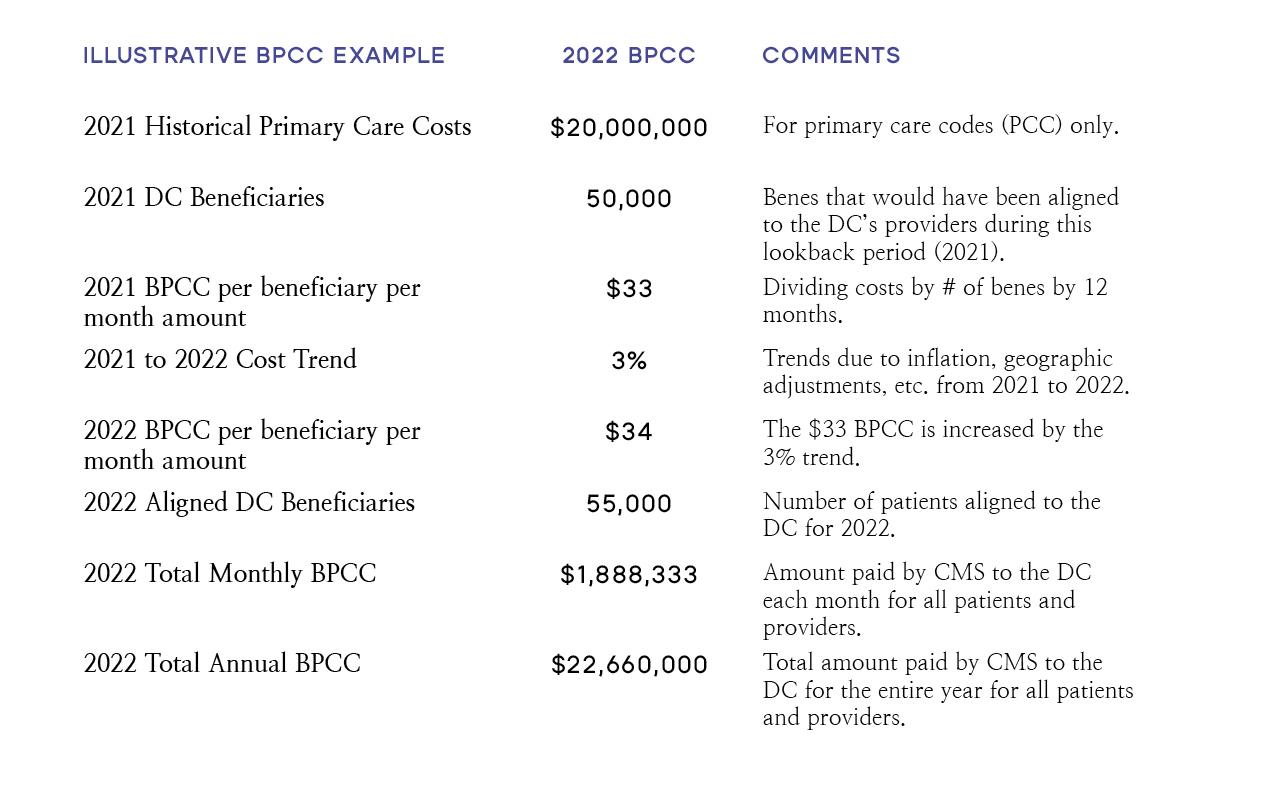
The Total Annual BPCC Amount typically ends up being about 2-4% of the TCoC and while primary care services account for less than 5% of total medical spend, PCPs directly influence more than 80% of downstream healthcare costs (hospital admissions, discharge disposition, post-acute care, etc.).
Short answer: Yes, because the monthly BPCC amount is based on historical spend, in other words, it’s based on how PCPs billed in the year prior.
Long Answer: It is intended to sufficiently fund PCPs’ aligned panel of DC beneficiaries based on the 2021 performance year medical expenditures. Remember, the BPCC is paid on a PBPM basis, (e.g., $34 PBPM), so if a PCP has more patients attributed to them in 2022 (100 patients) compared to 2021 (80 patients), their capitated payments will reflect the increase in patients ($34 BPCC amount * 100 patients * 12 months).
Short answer: Yes, but in a way that ties out financially.
Long answer: CMS will modify the 2022 BPCC amounts on a monthly basis. Some notable drivers of these adjustments include changes to:
- The count of current year 2022 aligned beneficiaries (e.g. the number of currently aligned patients will change over time with the addition of voluntarily aligned patients or future patient exclusions);
- The regional rate based on movement of beneficiaries during PY2022, e.g., a patient move from County A to County B since benchmark rates vary by county;
- The risk score of beneficiaries during PY2022 based on updated diagnostic codes, e.g., a patient acquires or resolves a new condition which will increase or decrease the benchmark;
- CMS's estimate of the rate of inflation of healthcare expenditure (the "USPCC trend") between the year prior to the performance year and the performance year.
There will be a significant impact to PCPs’ reimbursement for Primary and Qualified Evaluation and Management (PQEM) codes (i.e., primary care codes) beginning in January of 2022.
For all PCPs participating in a fully-capitated BPCC DC model:
- Billing: PCPs should continue billing CMS as they normally would for all claims for all DC patients. No changes here. It is critical to continue submitting FFS claims to maintain the capitation rates in future performance years.
- Reimbursement: Instead of being reimbursed by CMS for primary care claims, CMS will “zero out” their claims, meaning PCPs will receive $0 from CMS for their primary care services provided to DC aligned beneficiaries.
- Capitation: On a monthly basis, the DCE will pay each PCP their capitated payment for their DC-aligned beneficiaries, whether or not a PCP sees all or none of their aligned beneficiaries.
- For example, if a DC patient does not see their PCP during that month, the DCE will still reimburse the PCP the capitated amount for that patient.
- Shared Savings Revenue: PCPs have the opportunity to bear and capture value from the DC risk model by sharing in the cost savings that they generate from high-quality, cost-effective care. While shared savings are not paid out monthly like BPCC, PCPs will be rewarded about six to nine months after the performance year ends (e.g. Q3 2023).
The value of capitation is to provide PCPs with more consistent, predictable monthly revenue so they can dedicate more of their time managing the patients who need them most. Paying PCPs a fixed capitated payment each month will reduce unnecessary utilization, increase quality of care, and lower the overall cost of healthcare. Dedicating more time to the highest-risk patients will lead to better patient outcomes, especially in the costly post-acute care setting (e.g., reduced skilled nursing facility utilization).
Direct Contracting is the most innovative Medicare model ever launched by CMS. Requiring capitation is necessary to encourage PCPs to shift away from traditional FFS compensation to value-based payment arrangements.
At Pearl, we believe that capitation is not only the future of reimbursement, but also the best, most tangible approach to fixing our broken and expensive healthcare system. We advise all of our PCPs to follow these simple tactics to excel in the DC model:
1. Provide Annual Wellness Visits as early in the year as possible for DC patients.
- This will enable identification of new chronic conditions and will capture appropriate risk adjustment to properly fund their panel.
2. Provide preventative primary care services for high risk patients with multiple chronic conditions.
- Proactive management of sicker patients will allow PCPs to identify issues sooner, thus lowering the likelihood of hospitalization, reducing cost of care and untapping shared savings for providers. If PCPs lower the TCoC for their patients, they will share in the savings they generate.
- Additionally, increased primary care services in the current year (2022) will lead to increased BPCC amounts for providers continuing in DC in the following year (2023).
3. Voluntarily align all Medicare FFS patients
- Retaining, or growing, a panel of patients on a go forward basis will ensure a more stable, or increased, monthly capitated amount.
For more help unpacking how Medicare’s Direct Contracting model works, check out these resources. Follow Pearl Health on LinkedIn or Twitter for regular insights in your newsfeed.