Background
As high-cost, high-need (HCHN) patients may have consistently high spend regardless of intervention, their spending may not be significantly impacted by a primary care provider’s attention. Pearl aims to capture the “rising-risk” patients whose spending can be impacted by a PCP’s intervention. These “rising-risk” patients are patients who may currently have moderate spending but are at risk of becoming HCHN patients within the next 6-12 months.
Risk prediction models are developed utilizing data from large population studies to predict the probability of future events. Machine learning can be applied to risk prediction models, using algorithms to learn from past data, find patterns, and make predictions about the future. Machine learning is particularly powerful as it has the ability to recognize patterns that humans may not see, creating more intelligent and accurate models compared to traditional statistical methods. In our case, we can use claims data to identify patients at risk for becoming HCHN.1
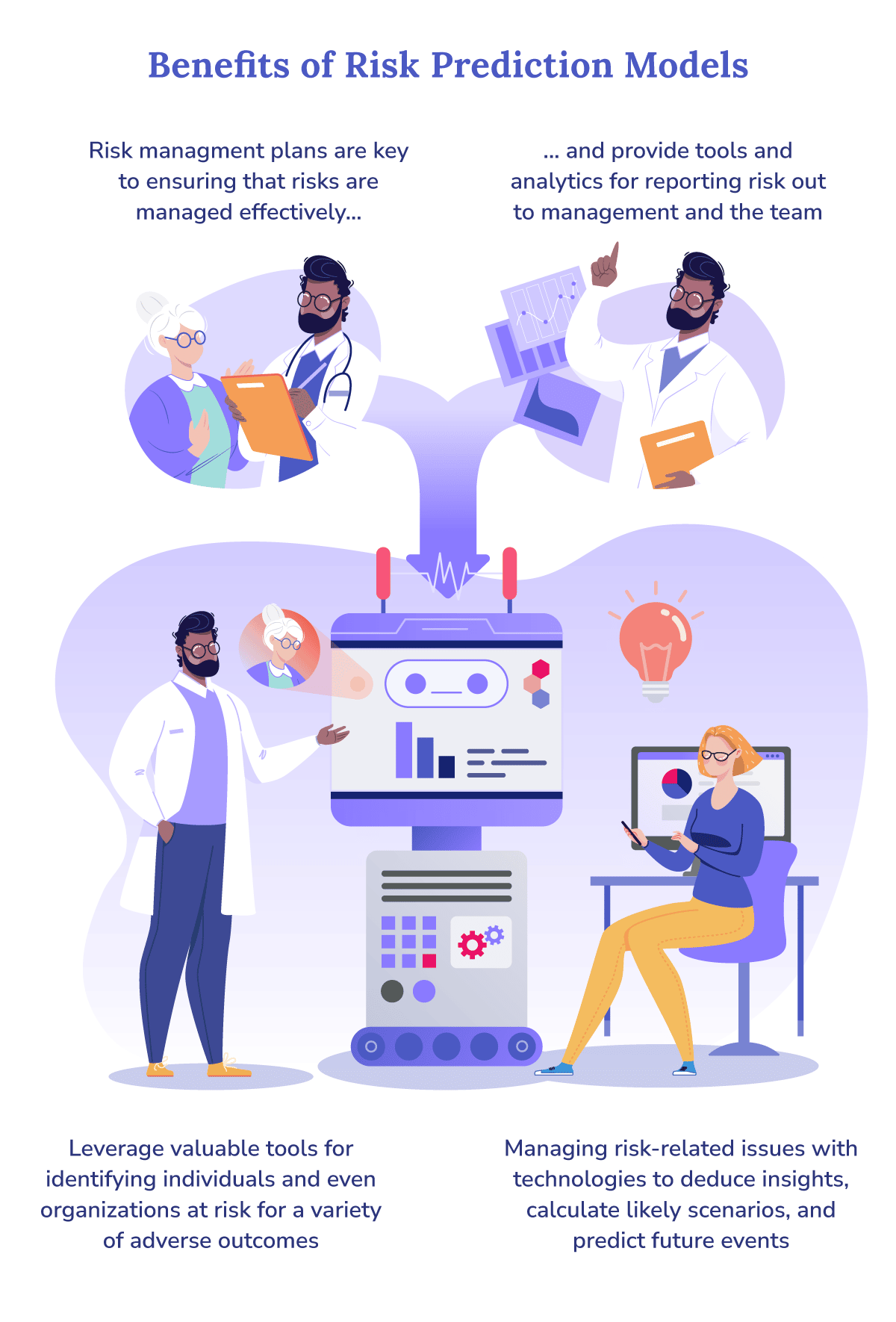
Adapted from “Everything you need to know about risk prediction models. Express Analytics.” Express Analytics. September 2, 2022.
Prediction Model Framework
Predicting future healthcare utilization and spending is essential in identifying patients who would benefit most from a PCP’s intervention. There are a number of models that can be used to predict this. These include standard models that have been well-documented, as well as more novel models resulting from current advancements in the field. Of these various models, there are a few key components common to all.
Data Processing and Predictors
Learning Algorithm
Interpreting Outcomes and Model Performance
Analysis of the model’s performance will be done by passing unseen data to the model. Model performance can be evaluated based on a few factors, including calibration (i.e. agreement between predicted and observed outcomes), classification (i.e. sensitivity and specificity), and clinical usefulness (i.e. if it is possible to make better decisions with the model than without).2
One challenge with these models is managing the risk of bias. In our case, we plan to use the Prediction model Risk of Bias Assessment Tool (PROBAST) to address this.5 PROBAST is a well-documented tool that has been previously utilized to identify any possible biases in participants, predictors, outcome, or analysis. Once any final tuning to the model has been made, the model is ready to make predictions.
What This Means for Pearl
With machine learning models, Pearl can forecast patient spending, identify those who are likely to become HCHN in the near future, and assist PCPs in making intelligent decisions about which patients may benefit most from their attention. This can contribute to solving the broader challenge of successfully intervening and improving patient outcomes — i.e., not just finding out who’s at risk, but figuring out how to help. Doing so will benefit both the PCP and the patient. With these models, Pearl can assist physicians in the clinical decision process and bring treatments to patients who need it most when they need it most. As a result, patient care may be significantly improved, as these models allow for earlier and more effective interventions.
Risk prediction models are incredibly useful tools that recognize the underlying patterns common to patients who will go on to become HCHN. At Pearl, these machine learning models allow us to look towards the future and target intervention on patients when it’s most impactful, improving outcomes and lowering spend.
Our Technology
- “Everything you need to know about risk prediction models. Express Analytics.” Express Analytics. September 2, 2022.
- Ursula de Ruijter MD, et al. “Prediction Models for Future High-Need High-Cost Healthcare Use: A Systematic Review.” Journal of General Internal Medicine, January 11, 2022.
- Chengliang Yang, et al. “Machine learning approaches for predicting high cost high need patient expenditures in health care.” BioMedical Engineering OnLine, November 20, 2018.
- Andrew W. Huang, et al. “Multivariable Prediction Models for Health Care Spending Using Machine Learning: A Protocol of a Systematic Review.” Diagnostic and Prognostic Research, March 24, 2022.
- Robert F. Wolff, et al. “PROBAST: A Tool to Assess the Risk of Bias and Applicability of Prediction Model Studies.” Annals of Internal Medicine, January 1, 2019.