Care management plays a central role in value-based care, helping primary care providers (PCPs) improve outcomes, support patients between visits, and reduce costly acute events. With the introduction of new Advanced Primary Care Management (APCM) codes in January 2025, the Centers for Medicare and Medicaid Services (CMS) has created a more flexible and inclusive reimbursement structure—one that builds on the foundation of traditional Chronic Care Management (CCM) and aligns with a broader vision for proactive, patient-centered care.
This post explores how APCM differs from CCM, what it means for primary care providers and accountable care organizations (ACOs), and how technology can support more scalable, efficient care management strategies under the new framework.
How APCM Broadens Access Beyond
Chronic Conditions
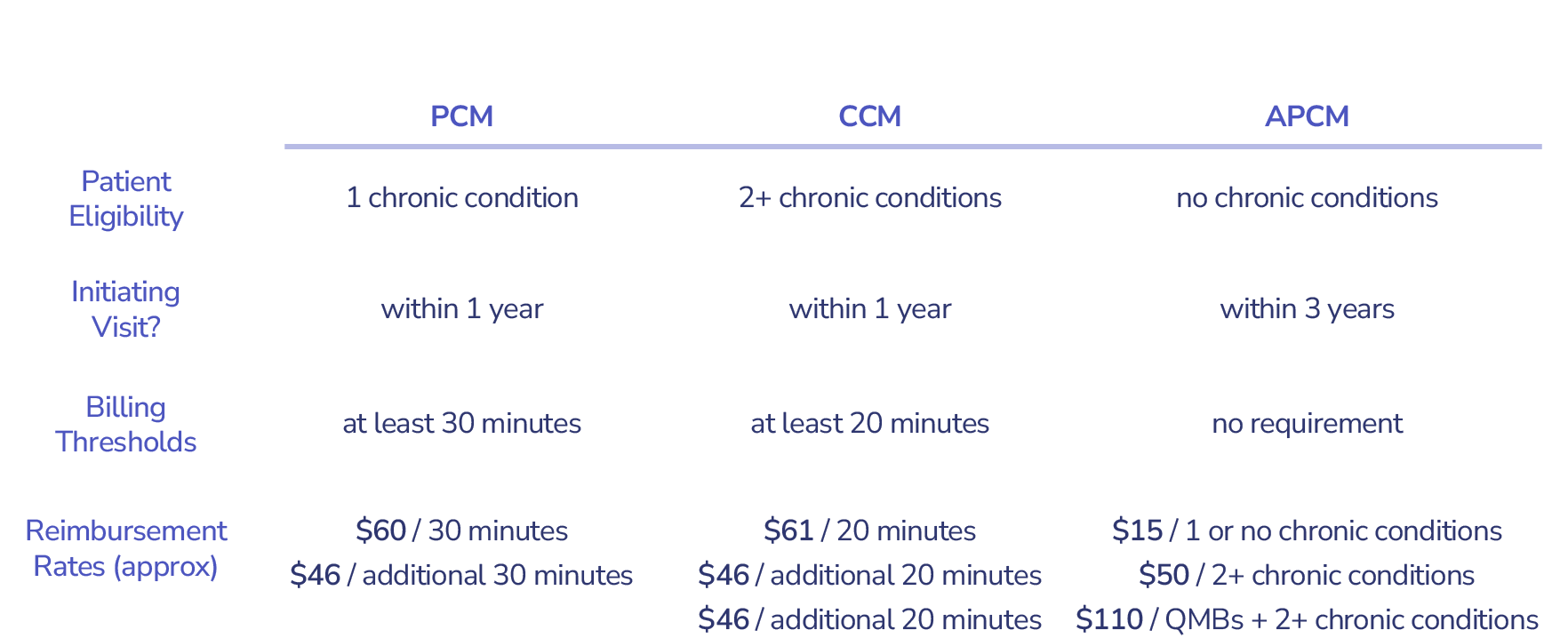
While any provider can deliver care management services, CMS defines specific requirements for when those services are billable. Traditional CCM has been a useful – but sometimes limited – tool, constrained by rules around patient eligibility and time-tracking requirements.
How Does APCM Compare?
- No chronic condition required: Patients can qualify for APCM even if they don’t have a diagnosed chronic illness—broadening access to high-risk individuals.
- No time-based documentation: Unlike CCM, APCM does not require a minimum number of billable minutes per month.
- No recent in-person visit needed: Patients do not need to have had a face-to-face primary care visit within the past 12 months.
A New Coding Structure That Supports Tailored Intervention
- Level 1 and Level 2 codes involve standard (20%) patient cost-sharing.
- Level 3 is designed for patients with more complex needs and does not require cost-sharing, reducing financial barriers to care.
New APCM Codes for Primary Care

To avoid duplication, the same practitioner cannot bill for both CCM and APCM for the same patient within a given month. However, another provider within the same practice may bill for a different, applicable service.
APCM Participation Requirements: A Shift Toward Accountability
To bill for APCM services, practices must demonstrate performance and population health management capabilities.
Participation in value-based care programs such as the Medicare Shared Savings Program (MSSP) or ACO REACH satisfies this requirement—further embedding APCM within CMS’ broader VBC transformation.
APCM Requirements
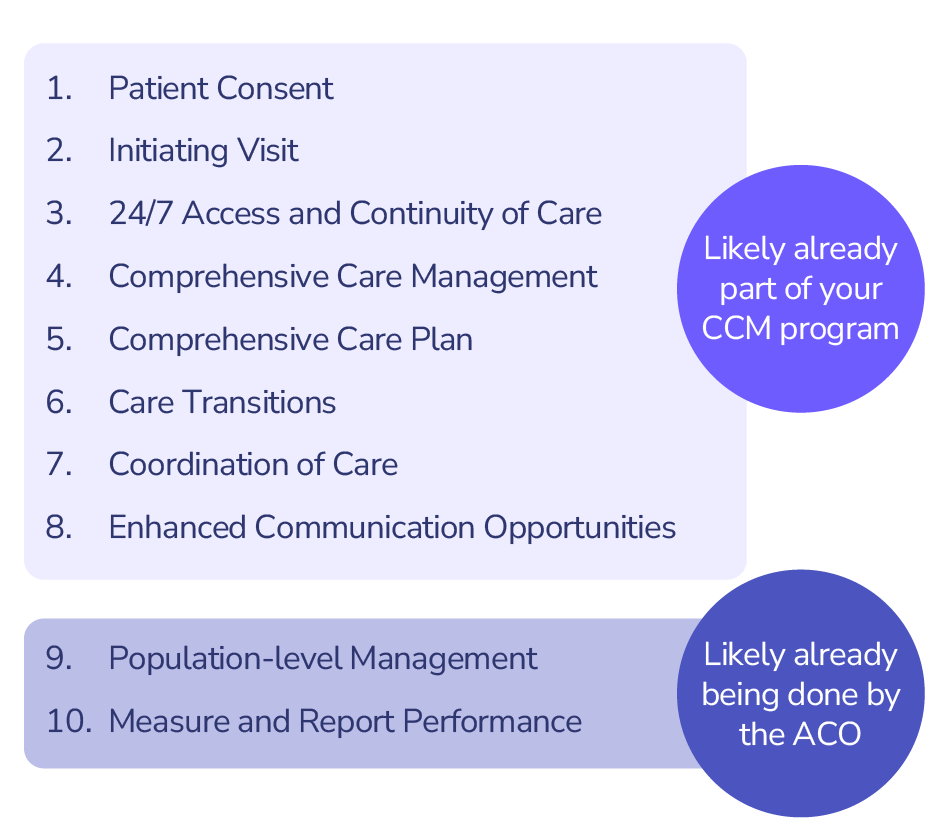
By linking reimbursement to participation in these models, CMS signals a clear policy direction: care management is not just a service—it’s a strategic lever for accountable care.
Why APCM Matters—and How PCPs Can Maximize the Opportunity
Pearl Health welcomes the addition of APCM to the care management toolkit. By introducing more flexible criteria and expanding the eligible patient population, CMS is enabling a more nuanced approach to delivering care between visits—especially for patients who would otherwise fall through the cracks.
But with more flexibility comes more complexity.
As eligibility expands and the types of reimbursable services grow, PCPs must navigate a more intricate decision tree: Which patients qualify for which services? When should APCM be used instead of CCM? What coding or cost-sharing considerations apply?
This is where technology becomes essential.
The power of Pearl’s proprietary software platform can help providers succeed with the new APCM codes. Our Signal Action Framework proactively surfaces patients who would benefit from different types of care management services, and the PCPs can use these recommendations to deploy their care management resources most effectively.
Looking Ahead
The introduction of APCM marks another important step in CMS’ journey toward scalable, accountable, and patient-centered care. By reducing administrative barriers and expanding reimbursement pathways, APCM makes it easier for PCPs to do what they do best: build trusted relationships, address problems early, and deliver whole-person care.
With the right technology and care management model in place, providers can unlock these new codes not just for reimbursement—but as a tool to improve outcomes and reduce total cost of care at scale.