Earlier this month, CMS released its proposal for the 2025 Medicare Physician Fee Schedule.1 A summary by America’s Physician Groups (APG) captured the moment well, commenting that the proposal “holds both promise and peril.”2
On one hand, the proposal includes several measures to improve care coordination, expand patient access to important primary care services, and advance value-based care. On the other hand, the proposal would decrease the Medicare physician fee schedule’s conversion factor by 2.8% in 2025, resulting in lower Medicare reimbursement for physicians.3 This would be the fifth consecutive year that the conversion factor decreased.4
Medicare physician pay has been plummeting for decades while operating costs have increased.5 When adjusted for inflation in practice costs, Medicare physician payments have effectively declined 29% from 2001 to 2024.6
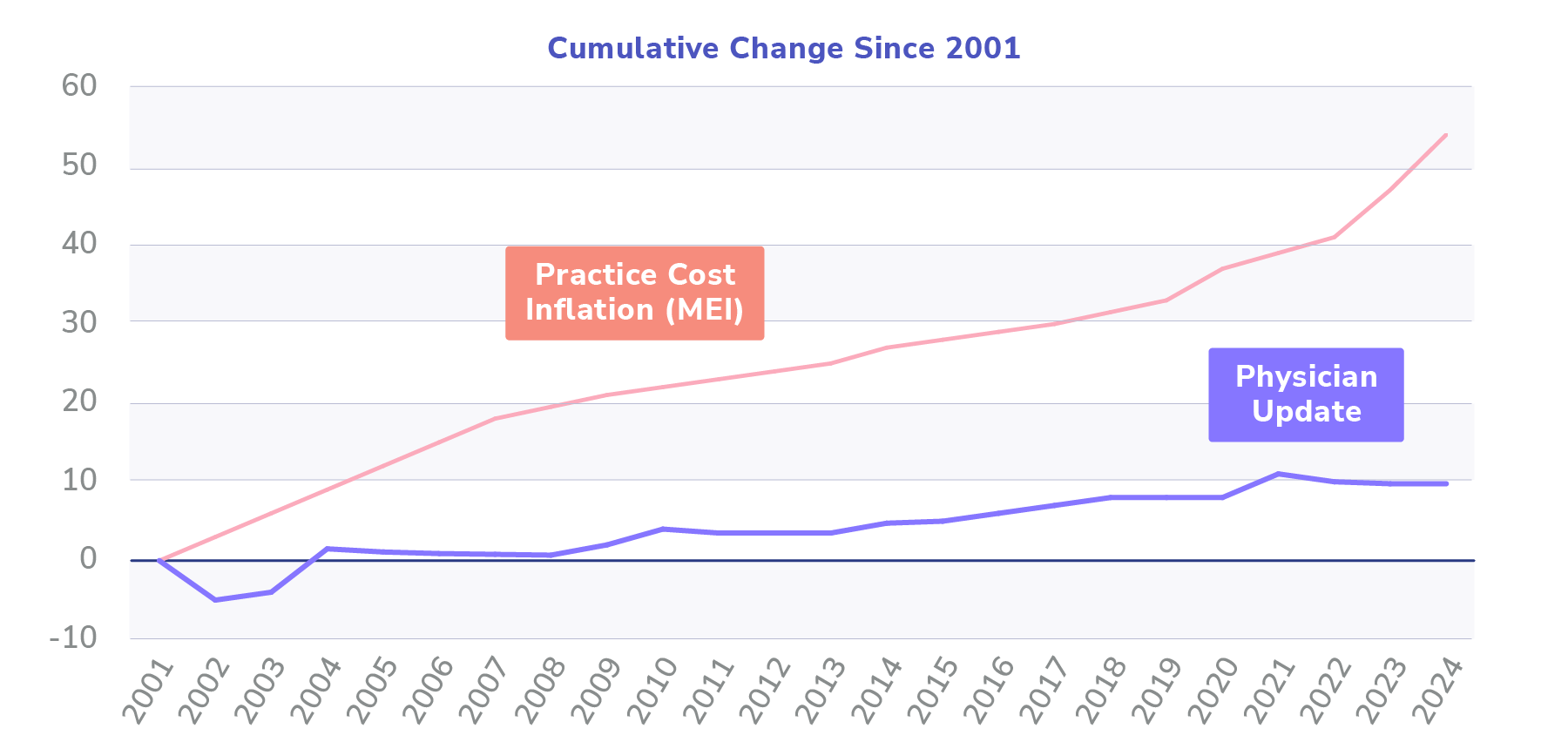
Chart adapted from visual in “Medicare physician payment is NOT keeping up with practice cost inflation.” American Medical Association, March 2024. Original sources: Federal Register, Medicare Trustees’ Reports, Bureau of Labor Statistics, Congressional Budget Office. Note: Updates from the Consolidated Appropriations Act of 2024 have been incorporated. As of March 2024.
Following decades of pay reductions, it is no surprise that the new proposed rule from CMS has sparked public outcry from many physicians and industry groups. In the hours following the CMS announcement, several organizations released statements protesting the proposal and urging Congress to intervene and increase assistance for struggling physicians, including: the American Medical Association (AMA), American Academy of Family Physicians (AAFP), Medical Group Management Association (MGMA), National Association of Accountable Care Organizations (NAACOS), Premier, and Society for Cardiovascular Angiography & Interventions (SCAI).7
“A 2.8% reduction to the conversion factor would be alarming in the best circumstances, but to propose doing so at a time when 92% of medical groups report increased operating costs and are otherwise struggling to remain financially viable is critically short-sighted,” said Anders Gilberg, MGMA Senior Vice President of Government Affairs. “Medicare physician reimbursement is on a dire trajectory and these ongoing cuts continue to undermine the ability of medical practices to keep their doors open and function effectively — the need for comprehensive reform is paramount.”8
We are still within the 60-day comment period for the proposed rule, which ends September 9, 2024,9 and many industry analysts believe that congressional action to provide relief seems likely.10 However, whatever the outcome of the 2025 Medicare Physician Fee Schedule, this proposal demonstrates the consistent trend of CMS moving toward lower physician reimbursements in fee-for-service payment models. Where, then, can primary care providers turn for relief?
Value-Based Care: Increasing Physician Revenue, Improving Patient Access
Notwithstanding the negative impact of a 2.8% reduction to Medicare reimbursements for physicians, the proposed rule does also include provisions that expand patient access to primary care services and create opportunities for providers to increase revenue through value-based payment models.
Many industry analysts view the 2025 Medicare Physician Fee Schedule proposal as the latest push from CMS as it seeks to realize its bold vision to transition all Traditional Medicare beneficiaries to accountable care relationships by 2030.11 12 This steady march toward participation in value-based care through accountable care organizations (ACOs) is essential for the future of our healthcare system. Physicians participating in value-based care programs with ACOs have been shown to have superior quality performance compared to other physician groups, and they have consistently generated year-over-year savings for the Medicare Trust Fund.
With the 2025 Medicare Physician Fee Schedule, CMS strengthens the Medicare Shared Savings Program (MSSP) by allowing eligible ACOs with a history of success in the program access to an advance on their earned shared savings to encourage investment in staffing, infrastructure, and additional services; it also proposes to further incentivize participation by ACOs in rural and underserved communities by adopting a health equity benchmark adjustment similar to that in the Realizing Equity, Access, and Community Health (REACH) Model.
For many primary care providers and organizations, models like MSSP and ACO REACH present opportunities to embrace more proactive care, align incentives with keeping patients healthy, and increase revenue for effectively managing care across diverse patient populations.
Partnering with Pearl
More importantly, these models will create incentives that are better aligned with outcomes and help to ensure that vulnerable beneficiaries do not slip through the cracks that often appear during otherwise non-reimbursable moments.
With the 2025 Medicare Fee Schedule proposal, CMS continues to make clear that innovative value-based care models, like ACO REACH, are a key part of their long-term strategy to transform the health-care system.
“Whole-person care means moving towards a health-care system that recognizes each unique aspect of a person and their wellbeing, including physical health, behavioral health, oral health, social determinants of health, and caregiving supports, and it all starts first with a foundation of primary care that can integrate these components,” said Meena Seshamani, M.D. Ph.D., Deputy CMS Administrator and Director of the Center for Medicare. “We are taking lessons learned from numerous CMS Innovation Center models to strengthen primary care teams and accountable care organizations, allowing them to better meet the unique needs of every person with Medicare.”
CMS Enrollment Deadline: August 1, 2024
The CMS enrollment deadline for MSSP and ACO REACH is rapidly approaching on August 1st. Faced with the prospect of lower Medicare fee-for-service reimbursements in 2025, many primary care physicians and groups are under pressure to evaluate the value-based care models most likely to help their organizations increase revenue next year and the ACOs best positioned to set them up for long-term success.
Yet, even those who have participated in value-based care with ACOs before may find it difficult to understand the potential tradeoffs of various newer models released by CMMI and the financial implications for their organizations.
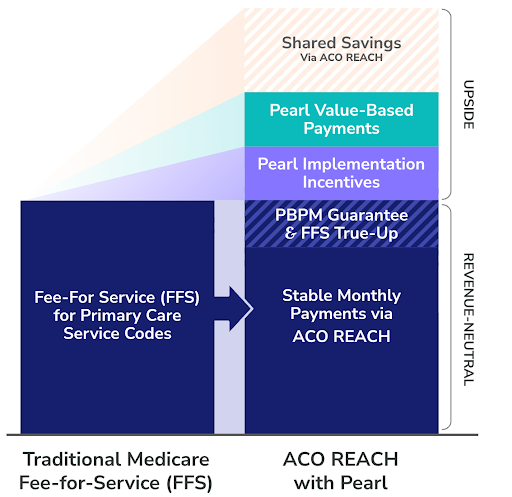
In ACO REACH, for example, providers have the opportunity to assume responsibility for coordinating the care of Traditional Medicare members in risk-sharing arrangements with the government. Over time, models like this will create incentives to deliver efficient, low-cost, and preventative care and facilitate more reliable and sustainable budgeting. They also have the potential to help PCPs stabilize and grow their practice revenue.
Setting aside the potential to increase Traditional Medicare revenue with models like ACO REACH, many organizations have limited experience in risk-bearing value-based care contracts, don’t fully understand the financial and/or operational implications, and aren’t confident in their ability to perform.
To succeed in the transition from volume to value, PCPs must take an increasingly central role in care delivery and coordination, and most practices lack the data and insights they need to proactively identify high-risk patients who may be slipping through the cracks. To make the most of emerging opportunities in value-based care, primary care organizations must avail themselves of the partnerships and enabling technology needed to succeed.
Whether your practice has deep experience in risk-bearing value-based care contracts or you are evaluating these programs for the first time, the Pearl Health team is here to help you understand the financial, administrative, and clinical considerations and tradeoffs associated with different models to help you maximize practice revenue.

Ready to See the Financial Impact?
Share a few details with us and receive a personalized analysis of how Pearl can work for your practice or network.
- HHS Proposes Physician Payment Rule to Drive Whole-Person Care and Improve Health Quality for All Individuals with Medicare, CMS, July 10, 2024.
- Proposed 2025 Medicare Physician Fee Schedule Holds Both Promise and Peril for Physician Groups, Says APG, APG, July 11, 2024.
- CMS’ proposed 2.8% physician pay decrease for CY2025 earns quick condemnation from docs, Fierce Healthcare, July 10, 2024.
- Another Medicare pay cut looms for physicians, Modern Healthcare, July 10, 2024.
- Medicare physician pay has plummeted since 2001. Find out why. American Medical Association, June 17, 2024.
- Medicare physician payment is NOT keeping up with practice cost inflation. American Medical Association, March 2024.
- Why Industry Groups Are Decrying CMS’ Physician Fee Schedule Proposal, MedCity News, July 10, 2024.
- MGMA statement on proposed 2025 Medicare Physician Fee Schedule, MGMA, July 10, 2024.
- HHS Proposes Physician Payment Rule to Drive Whole-Person Care and Improve Health Quality for All Individuals with Medicare, CMS, July 10, 2024.
- Yet Another Cut: Physicians Lose The Fee Schedule Battle Again, Hospitalogy, July 11, 2024.
- Yet Another Cut: Physicians Lose The Fee Schedule Battle Again, Hospitalogy, July 11, 2024.
- Innovation Center Strategy Refresh, CMS, 2021.
- HS Proposes Physician Payment Rule to Drive Whole-Person Care and Improve Health Quality for All Individuals with Medicare, CMS, July 10, 2024.



