Medicare beneficiaries with multiple chronic conditions are particularly vulnerable — the burden of comorbid conditions can compromise their health, making them more susceptible to complications that can lead to an unplanned hospital admission.1 These unplanned hospital admissions can expose patients unnecessarily to communicable diseases and often take a heavy emotional and financial toll on patients and their families. In addition, such admissions impose significant strain on the healthcare system overall. These patients tend to experience less coordinated care, with more complications and poorer outcomes, at a greater cost.
This impact may explain why CMS chose to include All-Cause Unplanned Admission for Patients with Multiple Chronic Conditions (UAMCC) as one of only four quality measures for ACO REACH — making the prevention of these admissions key to succeeding in the model.
At Pearl, we are focused on enabling our PCPs to improve outcomes and avoid preventable admissions when possible. To that end, we’ve recently added a new predictive algorithm to the Pearl Platform, which enables us to help identify patients with multiple chronic conditions who warrant proactive attention, as they may be at risk for an admission that could potentially be prevented.
Why This Approach?
Among other difficulties, patients with multiple chronic conditions often are at increased risk of rapid deterioration, require coordinated care amongst multiple specialists, and need more regular medication reconciliation. Research has consistently shown the positive impact of proactive, well-coordinated care in reducing these risks.2 The number of patients with multiple chronic conditions is large and ever expanding, however, making it difficult to know which patients to prioritize for proactive intervention.
We believe that PCPs are well equipped to work with patients to manage the collective impact of chronic conditions through regular check-ins and comprehensive care planning, but they may need help identifying and prioritizing the patients who are particularly likely to benefit from such intervention. With large patient panels and inconsistent or limited patient engagement, PCPs need an automated and targeted approach to identifying these patients.
Opportunity Identification
Pearl’s approach to any clinical opportunity follows a data-driven strategy. We first conduct extensive opportunity sizing analyses to determine whether there is likely to be:
- A prevalent problem
- That is clinically actionable
- In a way that will result in improved patient outcomes and cost savings
In the development of our predictive model, we tested how well the model would have performed in the past. This is known as backtesting. We do this by using historical data on patients to see if our model’s predictions match what actually happened to each patient. Our Data Science and Clinical teams then collaborated to compare the performance of our model with existing methods commonly used by clinicians, which are often based on studies and academic literature. This helps to ensure the actionability of these predicted admissions — i.e., as a clinician, if I knew my patient was at increased risk for an unplanned admission in the near term, then I could possibly change my care plan to prevent the visit. Our model performed well, achieving a c-statistic of 0.904. Further, if we compare the highest 3% of patients flagged by our model, it captured 175% more UAMCC admissions than a simple heuristic model based on the prior number of UAMCC admissions.
Bringing the Signal to Our PCPs
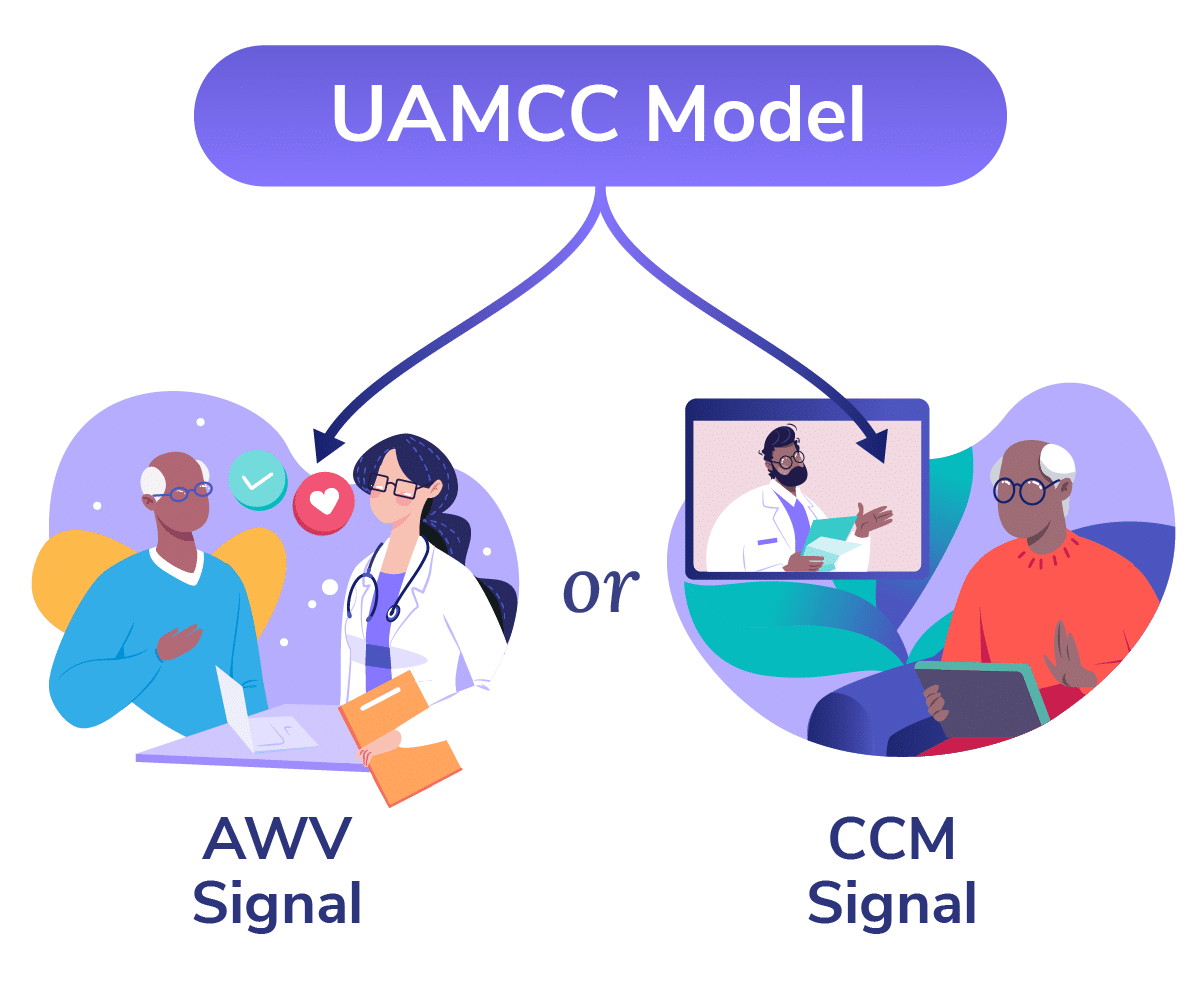
Our next step is to equip our partner providers with the power of our predictive analytics. Our focus is PCP enablement, and so we chose to leverage Pearl’s proprietary Signal-Action Framework platform to empower PCPs to proactively manage their patients with multiple chronic conditions at risk of unplanned admission.
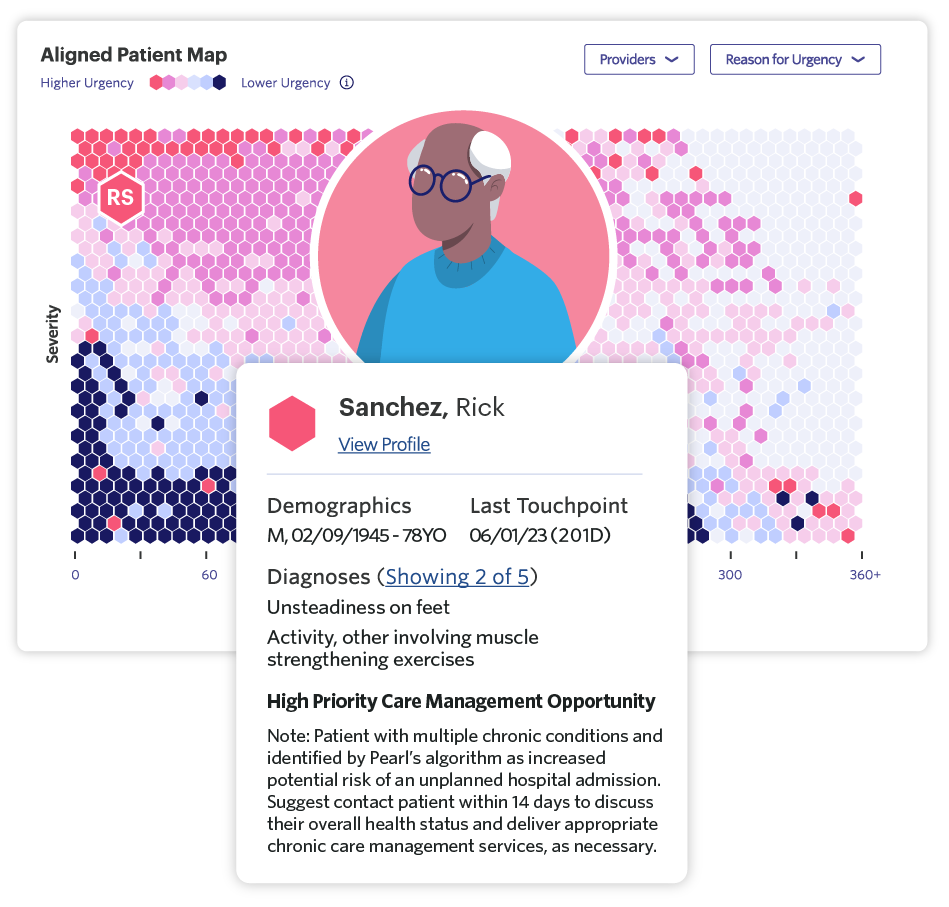
In the Pearl Platform, we have developed an urgency reason that will highlight patients with multiple chronic conditions whom our model has identified as being at particularly high risk for an unplanned admission and:
- Are due for outreach, possibly in the form of an AWV
- Would benefit from thorough review of their chronic conditions
- Would benefit from comprehensive care planning
Practically speaking, platform users will see patients alerted for “High Priority AWV” or “High Priority Care Management” opportunities, in an effort to make this as straightforward and clinically actionable as possible. Our goal is to empower proactive, well-coordinated care to help reduce vulnerable patients’ potential risk for unplanned admissions in the future — improving both patient outcomes and provider performance in ACO REACH’s UAMCC quality measure.
What’s Next?
As we continue to refine our predictive model, we are focused on monitoring and enhancing accuracy and fostering PCP engagement. Equally important, Pearl is committed to ensuring the likely clinical actionability of the model predictions.
Providing chronic care management (CCM) services in particular is crucial for promoting the ongoing health of patients with multiple chronic conditions. Looking forward, we’re exploring how to leverage the Signal Action Framework to prioritize patients who are most likely to benefit from CCM on an ongoing basis to improve overall health outcomes and reduce the risk of complications in this patient population. We’re excited to see the real impact this type of proactive, targeted prioritization will have for patients.
- Luciana Pereira Rodrigues et al., “Association between Multimorbidity and Hospitalization in Older Adults: Systematic Review and Meta-Analysis,” Age and Ageing, July 2022.
- From CMS’ Measure Information Form for UAMCC: “Several studies have shown that improvements in the delivery of healthcare services for ambulatory patients with MCCs can lower the risk of admission (Brown et al., 2012; Chan et al., 2012; CMS, 2012; Dorr et al., 2008; Edwards et al., 2017; Gabriel et al., 2017; Kuo et al., 2018; Krumme et al., 2018; Levine et al., 2012; Littleford & Kralik, 2010; Matzke et al., 2018; Ruiz et al., 2017; Sommers et al., 2000; Zhang et al., 2008). Demonstrated strategies include improving access to care; supporting self-care in the home; better coordinating care across providers; improved medication prescribing and dispensing strategies; and integrating social work, nursing, and medical services.”