Excerpt from the Top 50 VBC Thinkers Report
Medicare Advantage (MA) has been under pressure in recent years, as regulatory changes and financial adjustments placed new strain on the program. In 2024, plans reduced supplemental benefits, adapted to the transition from the V24 to V28 risk adjustment model, and faced heightened federal scrutiny—developments that reshaped economics across the market.
In 2025, however, there are signs of relief. CMS has announced a 5% rate increase for 2026 — representing more than $25 billion in additional payments¹ — while the risk model transition is nearing completion. Together, these updates suggest the MA landscape is stabilizing after a period of recalibration.
The following excerpt comes from Pearl Health’s annual Top 50 Value-Based Care Thinkers report, which highlights the leaders, trends, and ideas shaping the future of value-based care. This section examines how the MA reset is influencing payer-provider partnerships and what it signals for the broader shift to value.
Medicare Advantage: 2025 Market Reset
Medicare Advantage plans faced significant challenges throughout 2024 and early 2025, with widespread benefit reductions for the first time in over a decade². For dual-eligible plans, total value decreased by approximately $9.50 per member per month from 2024 to 2025³. Across all Medicare Advantage plans, supplemental benefits declined significantly, with reductions in over-the-counter allowances (from 85% to 73% of plans), meal benefits (from 72% to 65%), and transportation services (from 36% to 30%).⁴
Plans navigated CMS’s transition from the V24 to V28 Hierarchical Condition Category (HCC) model—projected to decrease MA risk scores by 3.12% while generating $11 billion in net savings to the Medicare Trust Fund—and intensified government oversight through expanded federal audits, which scaled from approximately 60 plan audits annually to auditing all eligible MA contracts, and DOJ investigations into alleged broker kickbacks.⁵ These pressures contributed to more than 1.8 million Medicare Advantage members being required to choose new plans for 2025 as carriers discontinued products or exited markets entirely.⁶
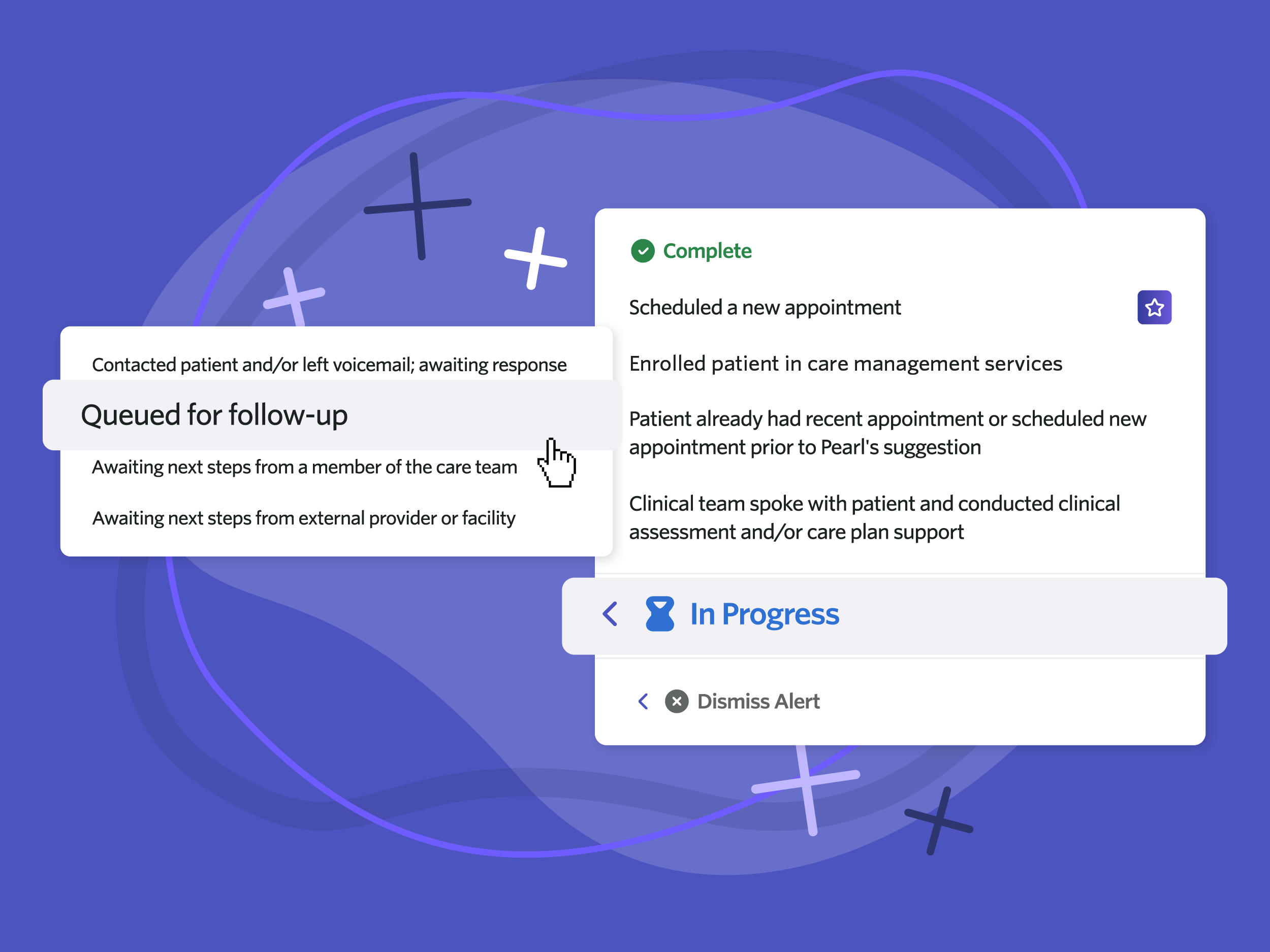
These regulatory pressures forced MA plans to fundamentally shift from growth-focused benefit expansion to sustainable partnership-driven approaches that emphasize operational excellence and demonstrable health outcomes. Rather than competing primarily through benefit enhancement, successful MA plans increasingly focused on partnerships with provider organizations that could demonstrate actual risk management capabilities and clinical excellence under intensified regulatory scrutiny. This strategic realignment creates significant opportunities for provider-led VBC organizations that can demonstrate sustainable population health management capabilities, as MA plans increasingly value partners who can help them manage complex populations effectively while maintaining clinical outcomes under regulatory scrutiny.
Despite these recent headwinds and strategic shifts for MA plans, recent policy developments signal potential relief: CMS announced a 5% rate increase for 2026—representing over $25 billion in additional payments to plans.⁷ This rate adjustment, combined with the completion of risk model transitions, suggests that, while the MA market has undergone a period of significant adjustment, there are emerging signs of stabilization and potential recovery. Industry observers view this as a foundational reset that positions Medicare Advantage for more sustainable growth, with successful plans emerging as those that can balance regulatory compliance, clinical excellence, and financial discipline. This strategic realignment ultimately reinforces the broader shift toward value-based care models, as MA plans seek provider partners who can deliver on the promise of better outcomes at lower costs.
Explore the full 2025 Top 50 Value-Based Care Thinkers report to see how leaders across healthcare are navigating Medicare Advantage, provider-led risk, and the future of value-based care.