If primary care’s time has come, why doesn’t it feel like it?
That’s one question we explored in Pearl’s Primary Care Pulse Report. After collecting survey responses from more than 200 physicians, conducting follow-up interviews, and exploring secondary research, we learned a great deal about the challenges PCPs face in today’s healthcare system. We explored one challenge, the epidemic of PCP burnout, in a recent blog post, and today will dive into another — physician pay.
A Broken Financial System
Multiple studies have shown substantial ROI on primary care investments, including one finding that every dollar invested in primary care saves $13 in downstream costs.1 Looking beyond the fiscal lens, primary care also offers substantial clinical benefits worth investing in to improve the health of our nation.2 3 Despite these facts, the average PCP makes 30% less per year than the average specialist,4 and according to the Brookings Institute, that pay gap is the single biggest motivator for those who choose to specialize.5
Shortchanging primary care pay is a problem for individual physicians and the system as a whole, with one downstream effect being a growing PCP shortage that is expected to reach between 18,000 and 48,000 by 2034.6 That means worse access to preventive care, sicker patients, and accelerating healthcare spend.
While we have known about the challenge for some time, the question remains: what can be done?
Increasing Pay & Improving Patient Outcomes
Through Value-Based Care
First, the bad news: Our Primary Care Pulse Survey reaffirmed the issues outlined above, with only 1 in 5 PCPs reporting that they feel fairly compensated.7 Even worse, respondents felt undercompensated and ill-equipped to provide the type of whole-person care that draws so many physicians to primary care in the first place. Only 3 in 10 PCPs reported feeling that their pay allows them to provide holistic patient care.
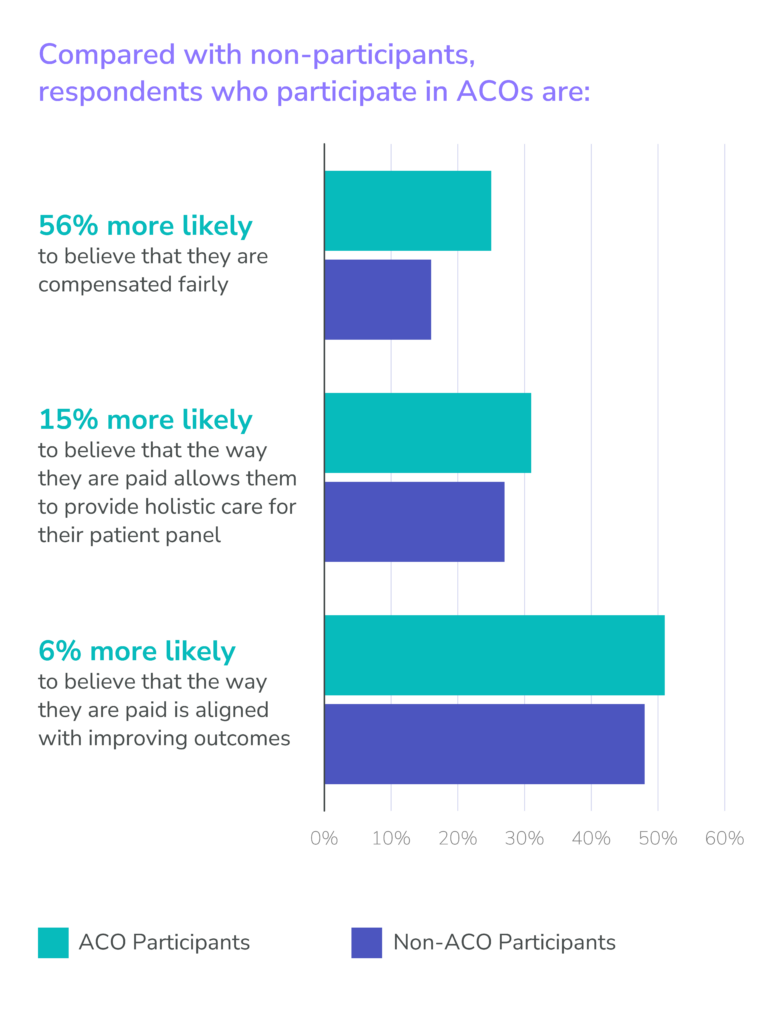
In brighter news, our survey also highlighted the promise of value-based care in reversing the trend around PCP pay. Compared with non-participants, those who participate in value-based care through Accountable Care Organizations (ACOs) are 56% more likely to believe that they are compensated fairly and 15% more likely to believe that the way they are paid allows them to provide holistic care for their patient panel.8
This improvement is a major step in the right direction, and at Pearl, we strongly believe in the promise of value-based care models like ACO REACH and the Medicare Shared Savings Program (MSSP). However, we also believe it is important to acknowledge that today’s value-based care models and programs represent a silver lining, not a silver bullet, to the challenges faced by PCPs.
Not all value-based care options offer the same earnings potential, and actually realizing that potential requires providing high-quality, proactive care to an entire patient panel. This represents a major shift from the fee-for-service model of focusing primarily on the patients in a doctor’s waiting room, and is one of multiple potential stumbling blocks for those transitioning to value. The promise is real, but so are the obstacles holding back many PCPs from making the leap.
Ready to learn more about the challenges and opportunities facing PCPs today across burnout, compensation & payment models, and value-based care adoption? Download the full Primary Care Pulse Report below.
- Medical Economics, “Delivering Value in Healthcare Starts With Increased Primary Care Investment,” August 2018
- Jama Network, “Quality and Experience of Outpatient Care in the United States for Adults With or Without Primary Care,” January 2019
- BMC Primary Care, “Primary Care Visits Increase Utilization of Evidence-Based Preventative Health Measures,” July 2020
- Medscape, “Physician Compensation Report,” 2023
- Brookings, “We Need More Primary Care Physicians: Here’s Why and How,” July 2019
- Association of American Medical Colleges, “The Complexities of Physician Supply and Demand: Projections From 2019 to 2034,” June 2021
- Pearl Health, “Primary Care Pulse 2023 Report,” 2023
- Pearl Health, “Primary Care Pulse 2023 Report,” 2023