The Crisis of Late-Stage Intervention
Medicare’s approach to end-of-life care reflects a fundamental misalignment between patient needs and healthcare delivery. Despite decades of evidence supporting early palliative intervention, we continue to witness a troubling pattern: palliative care arrives as an afterthought, often in the final days when suffering could have been prevented months earlier.
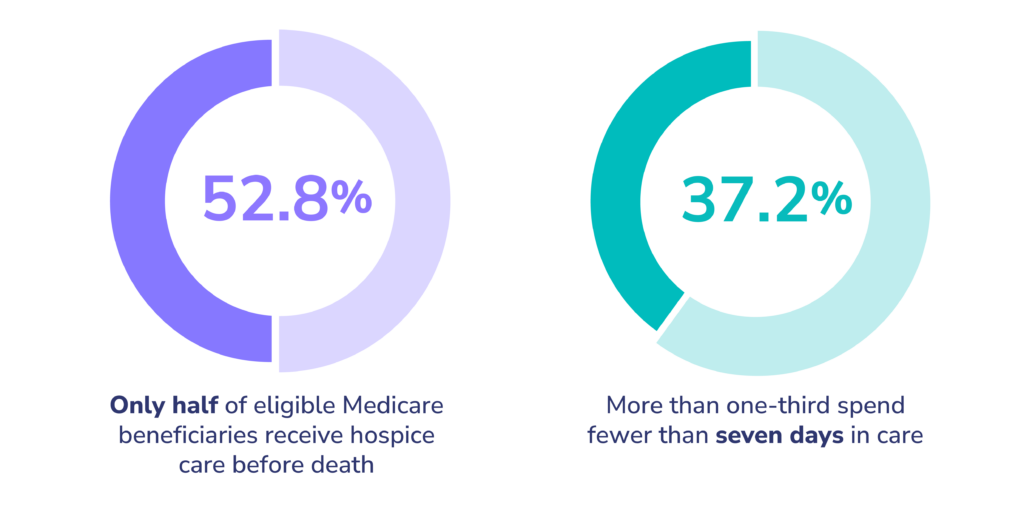
The statistics paint a stark picture. Only around half of eligible Medicare beneficiaries receive hospice care before death, with those who do enrolling with only days remaining—more than one-third spend fewer than ten days in care (CMS, 2025 Hospice Monitoring Report). This delay perpetuates unnecessary suffering while driving up healthcare costs through aggressive, often futile interventions that may contradict patients’ actual wishes.
As physicians working within technology-enabled Accountable Care Organizations (ACOs), we have both the opportunity and responsibility to fundamentally reshape this paradigm. The evidence is clear: early, inclusive palliative care isn’t just compassionate medicine—it’s essential for delivering quality care in our aging society while containing escalating costs.
The Clinical and Economic Case:
Evidence-Based Outcomes
Recent research continues to reinforce what the landmark Temel study demonstrated over a decade ago: early palliative care integration yields profound clinical benefits. A 2024 randomized clinical trial published in JAMA Network Open demonstrated that patients with advanced cancer who received early integrated palliative care showed significant improvements in quality of life, symptom management, and self-management skills compared to standard care alone (Kang et al., JAMA Open, 2024).
The economic argument is equally compelling. Medicare ACO data reveals that patients enrolled in home-based palliative care programs experience 51% fewer hospitalizations and are significantly more likely to utilize hospice services (70% vs. 43%), while incurring substantially lower costs in their final year ($27,203 vs. $36,089 average) (Lustbader et al., Journal of Palliative Medicine, 2017). These savings stem from preventing medical crises rather than responding to them—a shift from reactive to proactive care management.
This cost-effectiveness extends beyond individual cases. Risk-based payment systems are increasingly shaping the future of palliative care, with the palliative care market projected to experience significant growth as value-based care models recognize the return on investment in upstream interventions.
Addressing Inequities:
The Imperative for Inclusive Care
Palliative care’s benefits remain inequitably distributed across patient populations. Current utilization patterns reveal concerning disparities: hospice use among Medicare beneficiaries with dementia lags significantly behind those with cancer diagnoses (Teno et al., JAMA Network Open, 2022). Geographic and racial disparities further compound these inequities, with some communities experiencing disproportionately low hospice utilization and higher rates of aggressive end-of-life interventions.
Recent growth in Medicare Advantage plans offering home-based palliative care—with at least 157 plans providing these services as of 2023—represents progress toward broader access, but systematic barriers persist. An inclusive approach demands that we proactively identify and support patients across all serious illness trajectories, not just those in traditionally “hospice-aware” populations.
This includes expanding our focus beyond cancer to encompass patients with dementia, advanced heart failure, chronic kidney disease, and multiple chronic conditions—populations that often experience prolonged periods of functional decline where palliative interventions could provide substantial benefit.
Palliative care, in these contexts, is intended to orient treatments, referrals, and medical decisions towards the alleviation of symptoms, rather than the elimination of disease. As an example, an advanced heart failure patient may have their medications tailored to maximize quality of life, even if the underlying cause persists.
Transforming Identification and Referral:
From Reactive to Predictive
The traditional model of palliative care referral—waiting until curative options are exhausted or families request comfort care—fundamentally misunderstands the optimal timing for intervention. We must shift toward proactive identification systems that recognize patients who would benefit from palliative support months or years before crisis points.
Simple clinical tools like the “surprise question” (“Would you be surprised if this patient died in the next year?”) provide frontline clinicians with accessible screening mechanisms (Moss et al., Journal of Palliative Medicine, 2008). However, the real transformation comes through sophisticated predictive analytics that can identify at-risk patients before clinical deterioration becomes apparent.
Machine learning algorithms analyzing electronic health records and claims data can forecast which patients will likely benefit from palliative or hospice services, effectively creating early warning systems that augment clinical judgment (Avati et al, BMC Informatics, 2018). A technology-enabled approach to these complex cases often augments provider discretion, by revealing important patient/disease interactions that otherwise might be unrecognized. These tools don’t replace clinical decision-making but rather ensure that busy clinicians don’t miss opportunities for timely intervention.
Patient-Centered Care Models:
Meeting Patients Where They Are
Evidence consistently demonstrates that home-based palliative care (HBPC) programs reduce acute care utilization while improving patient and family satisfaction (Brumley et al., J Am Geriatr Soc, 2007). More importantly, these models honor patient preferences—most people want to spend their final days at home, and HBPC makes this possible while maintaining quality care.
HBPC programs also facilitate earlier hospice transitions. Research shows that hospice enrollments of 15 days or longer are associated with significantly lower Medicare spending and improved family outcomes (Taylor Jr. et al, Social Science and Medicine, 2007). This creates a virtuous cycle: earlier palliative care leads to timelier hospice referrals, which in turn improves both patient experience and cost efficiency.
The interdisciplinary nature of palliative care—incorporating physicians, nurses, social workers, chaplains, and other specialists—ensures comprehensive attention to physical, emotional, spiritual, and social needs. This whole-person approach addresses the complexity of serious illness in ways that traditional medical models often cannot.
Innovation Through Predictive Analytics: The Technology Advantage
Technology-enabled ACOs are uniquely positioned to implement sophisticated prediction and intervention systems. Pearl Health’s work within CMS’s GUIDE model exemplifies this potential, using predictive analytics to identify high-risk patients with dementia and trigger targeted interventions by primary care providers.

CMS' GUIDE Model
Discover how Pearl drives better outcomes, seamless care coordination, and stronger support for dementia patients and their caregivers.
This “signal-based” care model represents a scalable innovation that aligns patient needs with system incentives. By flagging patients before they reach crisis points, we can deploy appropriate resources proactively rather than reactively. The result is improved longitudinal management, reduced emergency utilization, and better alignment with patient goals.
Such systems require robust data infrastructure and clinical workflows that can respond to predictive signals, but the investment pays dividends through prevented hospitalizations, reduced family distress, and improved quality metrics.
The Path Forward: A Vision for Systemic Change
The future of Medicare’s serious illness care lies in fundamental transformation: shifting palliative care upstream, making it accessible to all who need it, and integrating it seamlessly into routine care delivery. This vision requires several key components:
- Systematic Screening and Identification: Every Medicare beneficiary with serious illness should be screened using validated tools and predictive analytics to identify palliative care needs early in the disease trajectory.
- Integrated Care Delivery: Palliative care should be available across all settings—hospitals, clinics, homes, and long-term care facilities—with seamless transitions between levels of care.
- Provider Education and Support: Primary care providers need training and resources to deliver basic palliative care interventions, with specialist consultation available for complex cases.
- Payment Reform: Value-based payment models should recognize and reward early palliative care interventions that improve quality while reducing costs.
- Cultural Transformation: We must reframe palliative care as a positive intervention that enhances quality of life rather than a sign of medical failure.
Conclusion: The Imperative for Action
The evidence is unambiguous: early, inclusive palliative care improves patient outcomes while reducing healthcare costs. For technology-enabled ACOs, this represents both an opportunity and an obligation. We have the tools—predictive analytics, integrated care models, and value-based payment structures—to deliver on this promise.
Real-world implementations, from Pearl Health’s GUIDE model to successful HBPC programs, demonstrate that this vision is achievable. What’s required now is the commitment to scale these innovations across Medicare’s beneficiary population.
As we face an aging population with increasing prevalence of serious illness, we cannot afford to continue the current pattern of late, crisis-driven palliative care. The time for transformation is now. By embracing early, inclusive palliative care as a cornerstone of value-based care, we can create a healthcare system that truly serves patients’ needs while stewarding resources responsibly.
The question isn’t whether we can afford to implement comprehensive palliative care—it’s whether we can afford not to. The evidence shows that timely, inclusive palliative care isn’t just compassionate medicine; it’s essential medicine for the 21st century.


