Medicare is one of the largest social systems in the world, by resources allocated and people served. It is a remarkable system that has scaled to almost a trillion dollars of expenditures in less than 60 years of existence. Keeping this system efficient and effective will be directly linked to the success of our nation and a harbinger for health systems across the world. Below, we share six predictions for the future of Medicare:
#1 Awesome Size and Scale
Demographics drive reality. Given US birth rates and population aging, the 65+ population will continue to increase as a percentage of overall population. In 1950, 65 year olds were 8% of the population, by 2050 they are forecasted to be 22% of the population.1 This shift, coupled with the increasing costs traditionally exhibited by medical innovations, will lead to significantly larger expenditures on behalf of Medicare. Over the same one-hundred year period, forecasters estimate growth from $5 billion to over $3 trillion of Medicare costs,2 one of the largest growing expenditure lines in human history. This substantial and consistent increase in growth can cripple economies and societies, but it also offers an opportunity for tremendous innovation and improvement of human life if those resources are properly utilized.
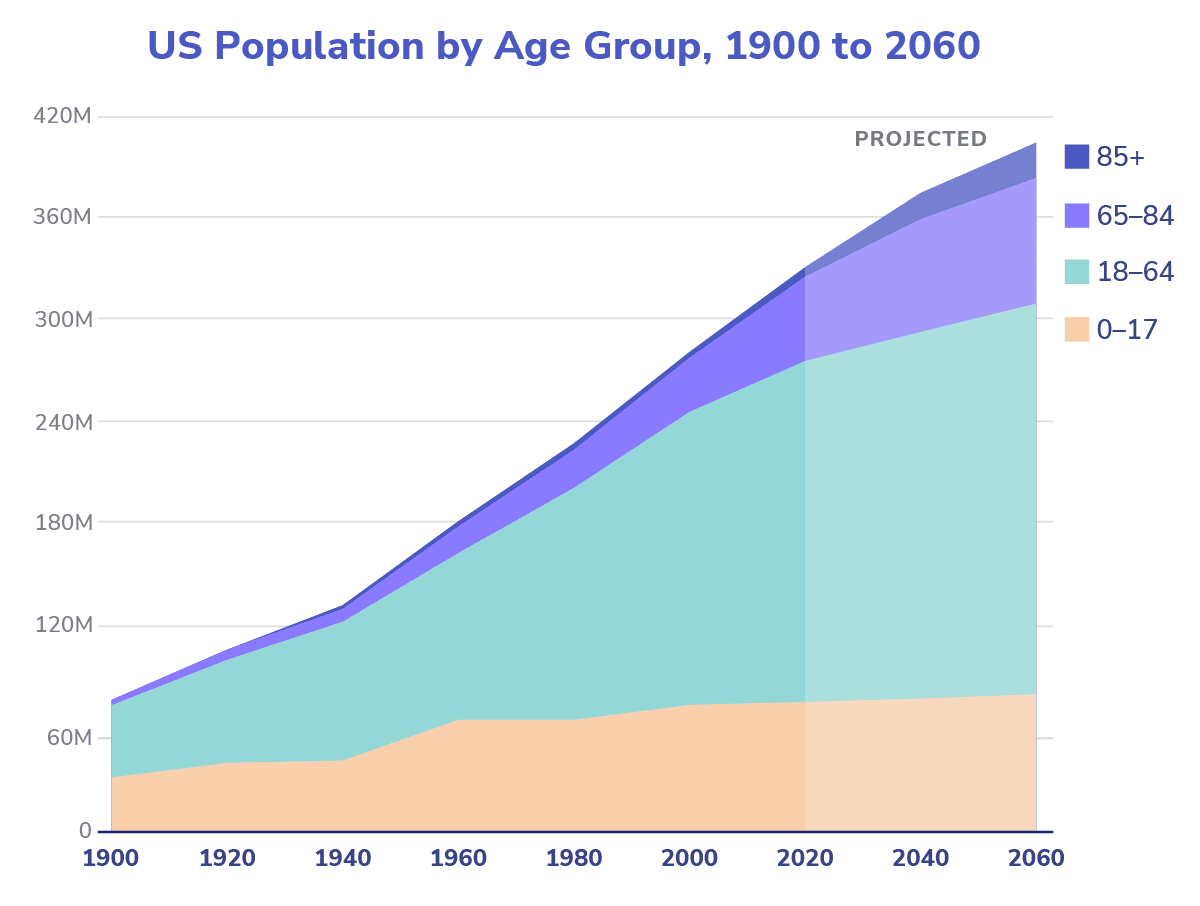
Source: Mark Mather and Lillian Kilduff, “The U.S. Population Is Growing Older, and the Gender Gap in Life Expectancy Is Narrowing,” Population Reference Bureau, February 19, 2020.
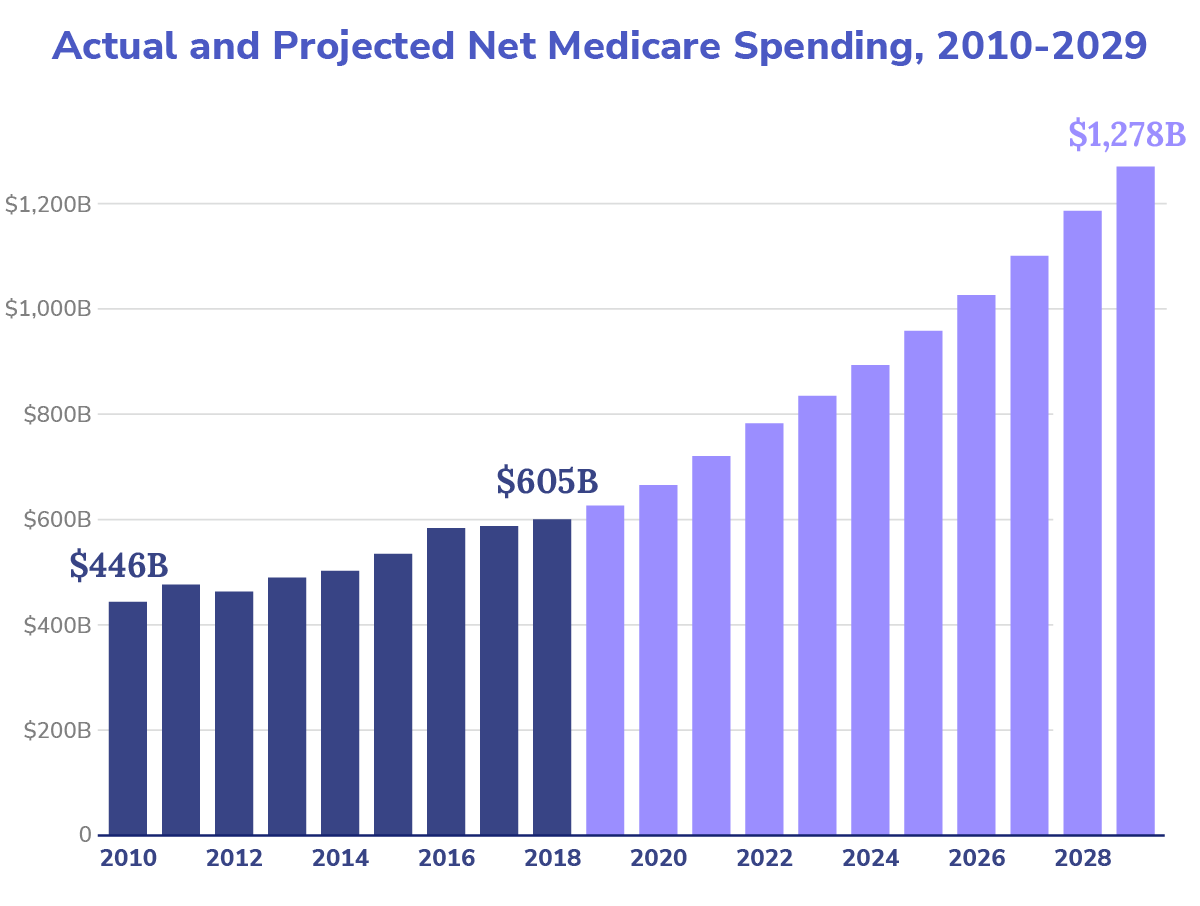
Source: Juliette Cubanski, Tricia Neuman, and Meredith Freed, “The Facts on Medicare Spending and Financing,” KFF, August 20, 2019.
#2 Integrated Concepts of Health Include Diet & Exercise
Any good study on the impacts of longevity and personal health invariably begins with basic concepts we all know well and learned early: the foundation of long-term health starts with diet, exercise, social interaction, and general wellness. As our massive system rotates from treating sickness to promoting wellness, it should be viewed as inevitable that we start to focus healthcare dollars on establishing better building blocks for population health. We have observed the impact of lifestyle improvements on many chronic illnesses. We have also seen the growth, via Medicare Advantage and ACOs, of better rebates and reimbursements for gyms, exercise programs, step goals, and other exercise-related activities. Although some of these investments can be hard to justify for private actors, they are easy to justify for population health leaders.
While Medicare will continue to fund therapies for established pathologies, we expect to see more consistent and integrated investments into evidence-based lifestyle improvements, the foundational building blocks of health. This can easily be accomplished by making healthier food and meals available to seniors and to be included in health benefits. Healthy habits, of course, work best when they begin early in life, and we anticipate more longitudinal alignment between commercial payors and CMS incentives, in order to ensure individuals are best-positioned when they join Medicare.
#3 Transportation and Social Interaction Enter Medicare
One of the great moral hazards of a social system where costs are distributed and borne by all is the unique fail point of expensive and avoidable individual cases. Examples include allowing someone with severe conditions to deteriorate because they can’t access proper healthcare or become isolated from family and friends. While the United States maintains a strong ethos of individualism and choice, it is irrational to allow significant failures in health outcomes borne by us all to occur needlessly. Increasing our healthcare infrastructure will necessitate including transportation and mobility as crucial components of a reliable delivery system.
The healthcare system will increasingly wire engagements to be opt-out vs. opt-in. Examples include automatic scheduling of appointments in care pathways with transportation as a bundled service. It is not cost-effective to allow logistical failures — a missed physician visit or drug pick-up — when they lead to emergency room visits or severe exacerbations of chronic conditions. Organizations like Lyft, Uber, Capsule, and others will increasingly integrate with medical providers to minimize fail points along an individual’s care journey. Other programs will seek to expand the reliability and complexity of home-based care, allowing services to come to patients, an inversion of the typical paradigm. Addressing mental and behavioral health drivers like loneliness and social isolation will increasingly be considered a core component of effective primary and preventative care. Organizations like Papa will increasingly move from novel to mainstream as a way of prolonging longevity and preventing chronic conditions.
#4 Early Detection and Predictive Preemption Through Better Data
As the social network generation ages, the concept of better data sharing to resolve avoidable health tragedies and prevent highly predictable health fail points will become expected. While the regime of HIPAA will likely remain, the lack of interconnectivity and dot connecting in healthcare is abhorrent. Interoperability in the coming years will be increasingly imperative, and we hope CMS will continue to encourage health record systems to use common data standards. The next generation of health policy leaders will reflect on the balance between personal privacy and data interoperability and will lean more heavily on data connectedness, as well as intelligent and automated intervention, to avoid unnecessary health failures across individuals and populations.
The amount of data that is currently available, combined with emerging concepts of social determinants of health, will heighten our capabilities not only to avoid tragic healthcare outcomes, but also to reduce the frictional costs of intelligent prevention and early detection. The largest drivers of healthcare expenditures (outside of end-of-life care) are failures of early detection and prevention.
Population health leaders know what to do and can deliver it once we enable a system that can give them the relevant information. While we will have to balance important concerns around privacy, the value we can unlock and the pain we can avoid by allowing better connectivity is growing to a truly awesome scale. Not allowing primary care physicians, nurses, and specialists to take action on this data to save ourselves and our loved ones will be considered unacceptable.
#5 Labor Service vs. Data Science as Healthcare
Increasingly, the concept of work in healthcare will shift. We will move from an industry that has historically considered labor hours, diagnoses, and prescriptions as the core work in the clinical setting to population health, data analysis, early detection and prevention (as seen above), and designing strategies for healthcare to address population health. As an example, the annual wellness visit (or even a check-up) is still seen as the base unit of work in healthcare. We anticipate this moving to digital experiences, with senior-first designs on ‘how to communicate to a population of seniors’, so they can participate in preventive screens and engage in wellness activities. This shift from a one-to-one to a one-to-many paradigm, where clinicians can design and improve healthcare outcomes for whole populations through workflows, communications, and technology, will enable us to get more efficiency from our clinical talent and drive better clinical impact in our populations, as opposed to thinking about healthcare through the lens of only a visit. Our regulators need to ensure that reimbursement models support and encourage this type of innovation, instead of relying on billable encounters as the base units of physician income.
#6 Family and Community Alliances
One of the most interesting byproducts of the US social safety net system has been the reduced agency families take with their loved elderly. While this is a generalized statement, it has manifested in how seniors live (outside multi-generational homes) and how they are cared for (family care vs. social security and Medicare). This has led to the reduction of connectivity and support of family and community alliances in driving health. As health becomes a community- and population-level problem, it will also increasingly tap into energy sources that are available but not fully utilized in family members and communities.
This will most easily manifest via the tools people are most comfortable with day-to-day, but it won’t be considered odd to link the health feeds of elderly loved ones to the devices of family members who want to subscribe, in order to help raise opportunities where clinical infrastructure will likely fail. Older concepts like “Life Alert” and “Help me, I’ve fallen and I can’t get up” may be replaced with timely and less extreme alerts around supporting a loved one who has missed an important appointment or a prescription or might benefit from engagement and activity due to loneliness. These same concepts can be woven into community-based groups who might start to experience key health interactions integrated into social experiences; imagine group therapy concepts, exercise classes, or cooking experiences to help drive and incentivize community and population health.
Controversial Prediction — Drug Blowback
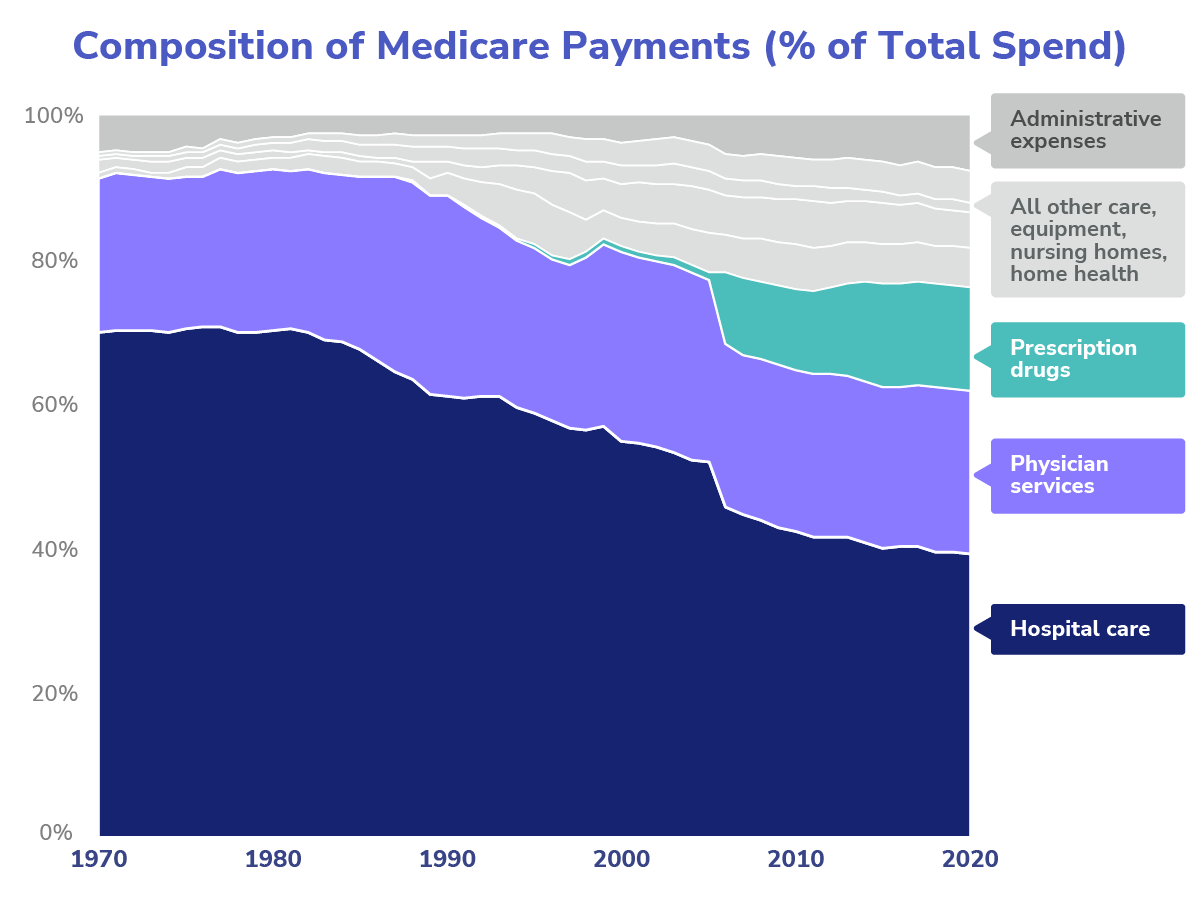
Source: Peter G. Peterson Foundation, “The Composition of Medicare Spending Over Time,” January 5, 2022; data: Centers for Medicare & Medicaid Services, National Health Expenditure Data.
I mentioned six predictions but I can’t help ending with a primary number and a controversial prediction. Nevertheless, I’m not sure this one will pan out to be true, as the emergence of pharmacological solutions to disease and ills could result in two polar worlds: one where we all have our own personalized medications (a modern “Brave New World”), and the other where there is a gradual but consistent rejection of the role of prescription medication in our lives. Much of it will hinge on the success we see in the predictions above and will likely still fall somewhere in the middle, but as physicians become more outcome- and population health-focused, there may well be a reassessment of the role we have allowed drugs to take with our seniors.
I was traveling between Bartlesville, Oklahoma, and Tulsa recently and my driver told me he was on 30 medications (15 he takes in the morning, 15 in the afternoon). He had a heart attack a decade ago, but he explained to me that he worked just to cover his drug costs and didn’t understand what they were all for; he noted that he was mentally tired of taking them. I’m 100% confident no individual physician today is looking over him and defragging his situation. I am also confident that several drug executives are quite satisfied.
Like most things in healthcare, the answer will be in between, but I am certain the growth in drug spend we have seen over the last decade is unsustainable and unhealthy for us all.
- Erin Duffin, “U.S. – seniors as a percentage of the population 1950-2050,” Statista. September 30, 2022.
- Veronique de Rugy, “Projected Medicare Spending Increases Over Time,” Mercatus Center, George Mason University. December 21, 2009.


