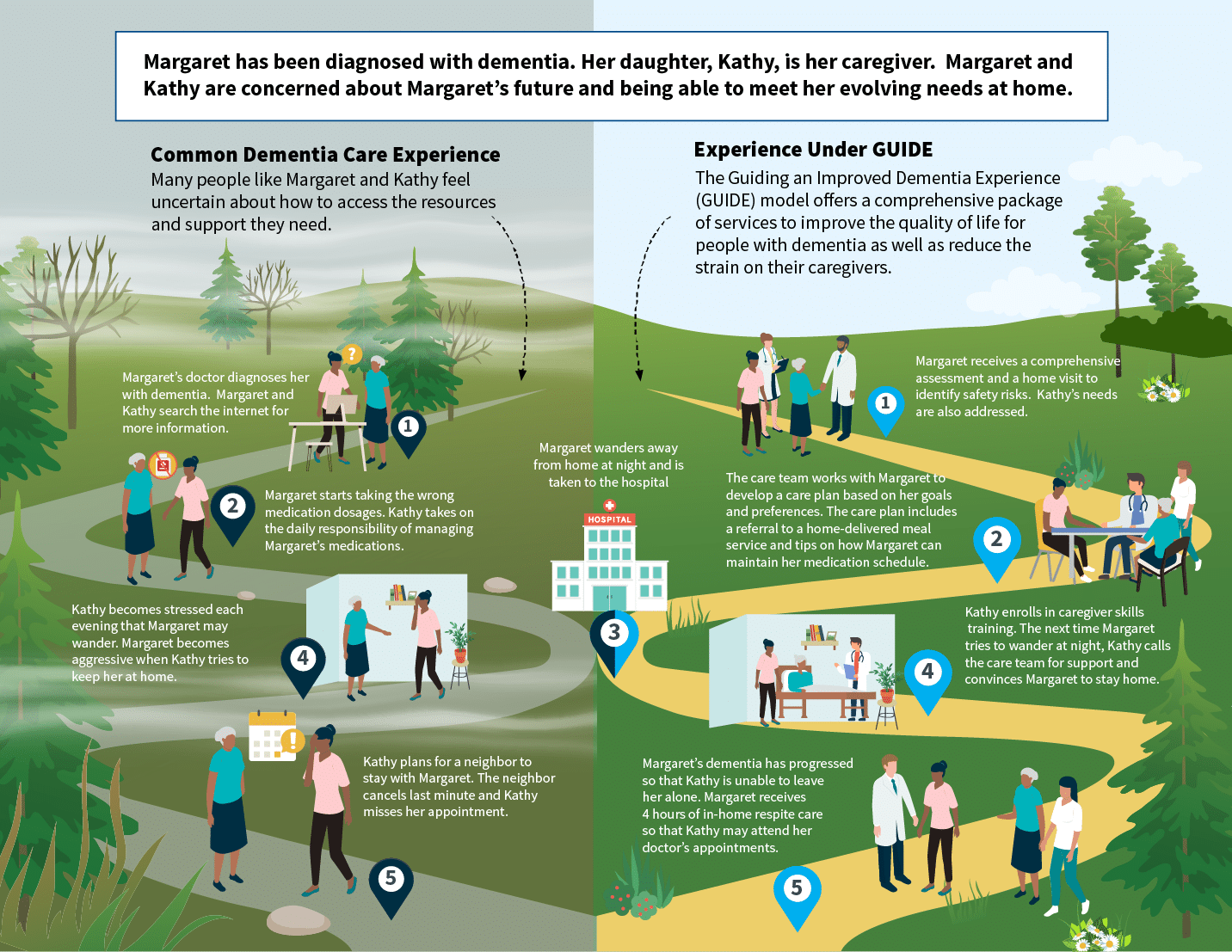
At Pearl Health, we’ve long recognized the widespread impact of dementia and the hurdles faced by both patients and their caregivers as they navigate this common and challenging condition. From the perspective of an accountable care organization (ACO), patients with dementia are very complicated, and they suffer disproportionately given challenges accessing and navigating care. Of equal importance, however, is the financial and health burden that impacts dementia caregivers – often the friends and family of patients. To this end, we have been preparing for the new “Guiding an Improved Dementia Experience” (GUIDE) program since its announcement by CMS in July of 2023. This model promises a comprehensive approach, providing much-needed care coordination and crucial support services for patients and caregivers. We believe in the transformative potential of this model to significantly enhance the lives of those dementia patients under the care of our provider partners.
What is the GUIDE Model?
Launching in July 2024, the GUIDE program stands as a voluntary nationwide alternative payment model (APM), offering traditional Medicare beneficiaries diagnosed with dementia an opportunity to enroll with a GUIDE participant. Organizations that become GUIDE participants will provide beneficiaries with an array of comprehensive assessments, care coordination, 24/7 support access, caregiver education, and respite care services. CMS is set to provide additional funds via monthly “Dementia Care Management Payments” and annual allowances for respite care, ranging from $4k to $6k in reimbursement to GUIDE organizations, all without any copayment from beneficiaries.
The GUIDE model is an especially interesting evolution of disease-specific APMs that have grown out of the Center for Medicare and Medicaid Innovation (CMMI). Unlike other APMs, the GUIDE model is purpose-built to be compatible with and supplementary to Medicare alternative payment programs (including ACO REACH). Beneficiary eligibility is largely unhindered by simultaneous participation in other Medicare programs, and the financial implications for ACOs are accounted for by CMS. GUIDE’s extended eight-year duration offers reassurance to interested providers, a significant departure from previous shorter-term APMs.
Given CMS’s substantial investment in dementia care, it’s imperative for ACOs and Primary Care Providers (PCPs) to closely monitor the unfolding landscape and its potential impacts on their respective dementia patients.
Implications for Primary Care Practices
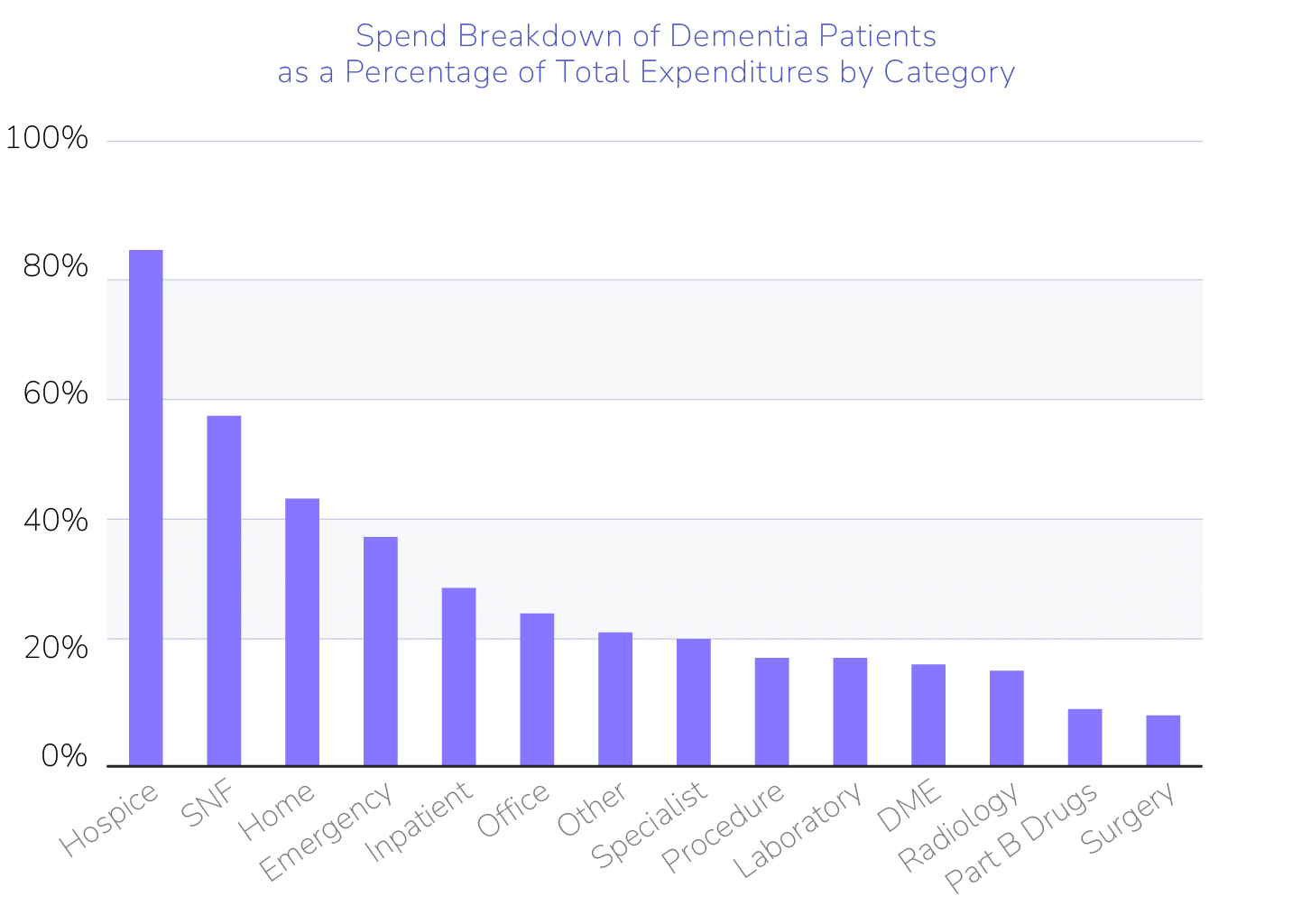
As front-line providers for Medicare beneficiaries, PCPs in the Pearl Community are well-acquainted with the complexities of identifying, diagnosing, and managing dementia. Academic research consistently shows that beyond performing initial cognitive screening and referring to a neurologist, PCPs are traditionally under-resourced in the long-term management of these patients. These challenges are accentuated by the outsized utilization and spending associated with dementia. At Pearl, dementia affects 14% of our population, yet accounts for over 30% of total medical expenditures. The need for an ACO-assisted playbook is clear, and we believe the GUIDE model is a key step forward.
Access to services provided by GUIDE organizations ensures that beneficiaries of Pearl PCPs receive timely and tailored care management crucial for mitigating the progressive impact of their condition. While the impact of these services is relatively untested, CMS and GUIDE organizations anticipate that this investment will yield long-term cost savings that will be reflected in Total Cost of Care models like ACO REACH — a hypothesis that will be subject to close monitoring.
Our analysis and discussions with potential GUIDE partners indicate that practice engagement will be critical to success. To realize the value of GUIDE, PCPs will remain pivotal in identifying eligible patients, facilitating patient enrollment with partnered GUIDE organizations, monitoring the quality of GUIDE services received, and integrating GUIDE care plans into the ongoing management of their patients’ comorbidities. These substantial tasks may overwhelm PCPs, and that’s where Pearl can help provide essential support.
Pearl’s Engagement with GUIDE
Pearl Health is well-positioned to leverage our analytical expertise and provider enablement platform to help PCPs maximize value from GUIDE. We are seeking to partner with a few leading GUIDE organizations capable of effectively implementing programs tailored to our beneficiaries. Our discussions with potential partners thus far have focused on geographical coverage, operational models, and team compositions for delivering CMS-required professional services.
Pearl’s strength lies in utilizing Data Science to prospectively identify beneficiaries at risk of under– or over-utilization and then signaling PCPs via our platform, ensuring optimal engagement. Upon identification in the platform, PCPs will be able to seamlessly prepare and refer patients to a contracted GUIDE partner organization that has an approach with meaningful quality and operational benefits. In order to help optimize outcomes, we continuously monitor enrollment and healthcare utilization trends across our PCP Community.
We will apply these same processes to help health system partners who are interested in directly applying to become a GUIDE participant. There are two tracks for enrollment, an established program track that starts in 2024 and a new program track that will start in 2025. Larger provider organizations may find direct enrollment an appealing way to reimburse qualifying existing care coordination efforts. While there are additional requirements, Pearl Health can help navigate these intricacies to facilitate successful enrollment and participation.
Concluding Thoughts
At Pearl Health, we’re eagerly anticipating the launch of the GUIDE program in July 2024. This innovative alternative payment model represents a leap forward in the effort to improve outcomes and reduce total cost of care for individuals with dementia. As primary care providers will continue to play a vital role in patient identification, enrollment, and ongoing management, Pearl is ready to enable PCPs by leveraging our analytics and collaborating with GUIDE organizations to ensure effective partnership. We’re excited to collaborate with provider organizations interested in navigating this transformative model to improve dementia care.
- For more information, see the National Library of Medicine