Why this approach?
We know that preventable ED admissions reflect both conditions that can be treated non-urgently and also deteriorations of poorly-managed chronic conditions. While ED visits due to non-urgent conditions are predominantly a patient education problem, we believe PCPs can play a vital role in preventing the latter problem. Too often, interoperable information is lacking, and PCPs are unaware of the patient movements driving outcomes in their population. Large patient panels and inconsistent patient engagement begs the need to equip PCPs with an automated and targeted approach to identifying these patients.
Opportunity Identification
- There is a highly prevalent problem
- The problem is clinically actionable
- Addressing the problem will result in improved patient outcomes and cost savings
Applying this framework to preventable ED utilization, we found that nearly 1/3 of our total ED utilization was preventable (prevalent and actionable) and a Per Beneficiary Per Month analysis found a massive cost savings opportunity for our ACO’s PCPs.
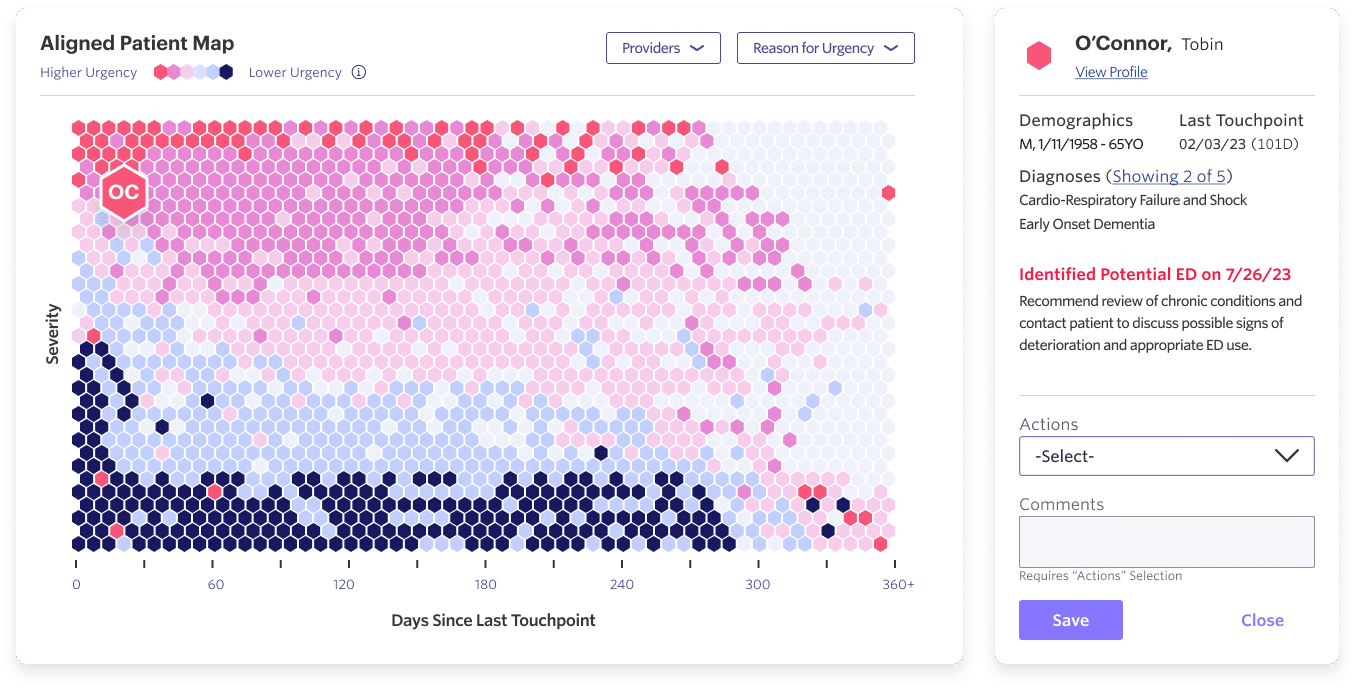
Once the opportunity was validated, our Data Science team focused on trying to predict future preventable ED admissions using historical patient activities. Our Data Science and Clinical teams then collaborated to ensure the actionability of these predicted visits — i.e., as a clinician, if I knew a patient was likely to have an ED visit in the next 90 days, then I could possibly change my care plan to prevent the visit.
Bringing the Signal to our PCPs
White Paper
Signal-Action Framework & Urgency Score
In this document, you’ll learn about the algorithm and signals that power the insights surfaced within the Pearl Platform.
Download White Paper
Signal-Action Framework & Urgency Score
For example, take a patient whose poorly controlled diabetes and asthma puts them at risk for ED overutilization, repeat prescriptions refill requests, and poor specialist follow-up. Our predictive model alerts this patient as top priority on the Pearl Platform for their PCP to discuss signs of decline and appropriate medication and ED use.
The Road Ahead
As we continue to refine our machine learning model, we are focused on monitoring and enhancing prediction accuracy and fostering PCP engagement. Equally important, Pearl is committed to ensuring the clinical actionability of the model predictions. One exciting avenue for this is the potential for collaboration with other healthcare vendors, such as Transitional Care Management (TCM) or home health providers. By combining our predictive capabilities with their services, we can amplify our efforts to reduce preventable ED visits by helping PCPs coordinate the right level of care at the right time in the right setting for the patient.
Pearl’s predictive algorithm represents a significant leap forward in addressing preventable ED visits. Through meticulous development and clinical validation, we have created a powerful tool that equips our PCPs with the insights needed to intervene proactively and provides our ACO with a repeatable framework for deploying similar predictive analytics in other clinical opportunities. Stay tuned for more!
- Weinick RM, Burns RM, Mehrotra A. “How many emergency department visits could be managed at urgent care centers and retail clinics?” Health Aff 2010;29(9):1630-6.
- Dowd B, Karmarker M, Swenson T, et al. “Emergency Department Utilization as a Measure of Physician Performance.” American Journal of Medical Quality. 2014;29(2):135-143.