Are you a PCP? Share Your Experiences in the Primary Care Pulse
At Pearl Health, we believe that primary care providers are key to America’s health. We also know first hand that the majority of PCPs today — from solo practitioners to providers in large multispecialty organizations — feel overworked, under-resourced, and inadequately rewarded in their efforts to deliver better care.
Our mission is to help primary care providers and organizations transition to value-based care models that allow them to increase practice revenue while delivering more proactive, whole-patient care. To that end, we’re always looking for ways to better understand the challenges and pressures that PCPs face in navigating the clinical, administrative, and financial realities of US healthcare. That’s why our team conducts an annual survey of primary care physicians: the Primary Care Pulse.
Through survey responses, follow-up interviews, and in-depth research, we identify the impediments and frustrations confronting PCPs in their daily work, as well as the opportunities they have for achieving deeper satisfaction in the practice of medicine, greater financial reward, and better outcomes and experiences for their patients.
Our 2023 Primary Care Pulse gathered the perspectives of more than 200 primary care providers across the country in practices of all sizes. In 2024, we’re collecting more responses, conducting more interviews, and sharing our data with practicing physicians to gather their feedback and insights on our findings.
We invite you to join us in this important research — your input helps us continue to nuance our understanding of what it’s like to be a primary care provider in the US today and helps us refine our approaches to helping PCPs and their patients thrive.
SURVEY OPEN
2025 Primary Care Pulse
Fill out this short survey and share your experience as a primary care provider
Findings from Our 2023 Primary Care Pulse
The need for value-based care is profound. With the Medicare trust fund on the verge of bankruptcy,1 an aging population,2 and healthcare costs steadily increasing,3 the US healthcare system is approaching a financial breaking point. Meanwhile, chronic conditions are rising in prevalence and severity,4 resulting in poor health outcomes that are often avoidable and exacerbating existing strains on the system.
In response to these unsustainable trends, our healthcare system is undergoing a massive shift from its traditional focus on acute care, specialty care, and high-volume utilization toward a system built around preventive care, holistic wellness, care management, and population health.
But value-based care won’t work unless primary care is central. Any model designed to improve outcomes and lower overall costs must depend on PCPs to engage patients with preventive whole-person care while monitoring their health for red flags or worsening conditions, and facilitating coordination, follow-up, and even the provision of appropriate social services.
That’s an impossible reach for most primary care physicians without aligned compensation, an infrastructure of support, and tools to practice medicine efficiently and effectively. In our 2023 Primary Care Pulse, only 3 in 10 PCPs responded that they believed their pay allowed them to provide holistic care; only 6 in 10 responded that they felt equipped to engage their panel in preventive care.
The PCPs who reported in our survey that they were actively participating in value-based care were 56% more likely to believe that they were compensated fairly and 15% more likely to believe that the way they are paid allows them to provide holistic care for their patients.
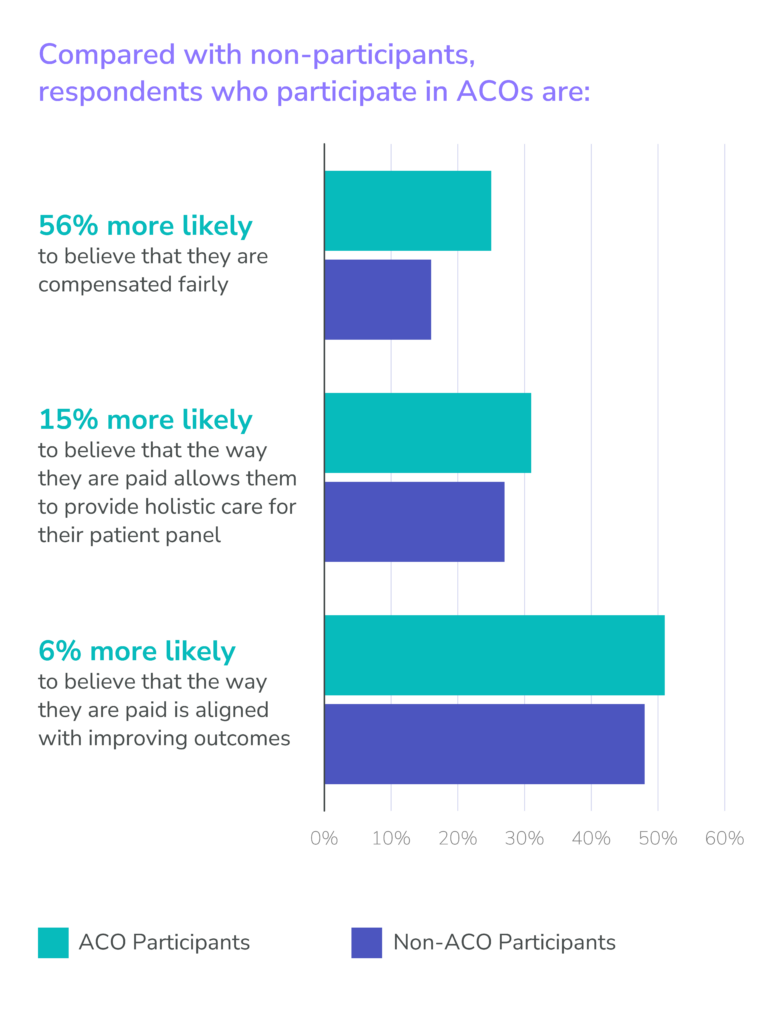
These numbers suggest that ACOs are one path toward a better future for primary care physicians — a future in which they are paid to practice medicine with their patients’ holistic wellness in mind. Yet, it seems that few PCPs today feel completely equipped to succeed in models that most view as the right path forward for our healthcare system.
While the PCPs who were aligned with accountable care organizations (ACOs) responded more positively in our survey than non-participants, many reported leaving early ACO models because of unrealized financial promises and overwhelming administrative demands. The majority of those respondents would still consider joining another ACO in the future, yet some remain concerned about financial risk, skeptical about benefits, and unaware of how newer models have evolved to address previous financial, administrative, and clinical challenges.
The Centers for Medicare and Medicaid Services (CMS) has set a goal to have all patients with Traditional Medicare in an accountable care relationship by 2030,5 and innovative value-based care models like ACO REACH offer powerful incentives that can help PCPs overcome obstacles in the transition to value-based care. At Pearl Health, we’re committed to equipping primary care providers and organizations with the information they need to make the most of these opportunities, the financial incentives to make the transition to value possible, and the insights and tooling they need to succeed.
Succeed In Value-Based Care With Pearl
- Peter G. Peterson Foundation, “Budget Basics: Medicare. Medicare Hospital Insurance Fund Surpluses / Deficits (% of GDP, 1970-2100).”
- U.S. Census Bureau, Population Estimates and Projections. Cited in U.S. Department of Health and Human Services, Administration of Community Living, “2020 Profile of Older Americans,” May 2021.
- Statista, “U.S. Health Expenditure as Percent of GDP from 1960 to 2021.”
- Wullianallur Raghupathi and Viju Raghupathi, “An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach to Public Health,” 2018.
- Centers for Medicare & Medicaid Services, “CMS Announces Increase in 2023 in Organizations and Beneficiaries Benefiting from Coordinated Care in Accountable Care,” January 17, 2023.