In Part II of the Value-Based Care Playbook, we outlined the three conceptual lessons that anyone seeking to embark in value-based care should understand. Here in Part III, we delineate tactics that will help providers set themselves up for success as they transition from fee-for-service to value.
Address the ‘Locality Conundrum’
We referenced the locality conundrum in Part II, but as a refresher: depending on where you are practicing, you may be especially exposed to the locality conundrum in healthcare — in other words, the inherently local delivery of many acute healthcare services can predictably generate anti-competitive forces and precipitate effective monopolies, making it harder to provide high-quality care at low cost. Providers can end up feeling trapped, as if they have no efficient partners in delivering care, and no ways to help their patients manage costs of necessary care.
With the right VBC partners and tools, providers can address the locality conundrum through:
- Increased access to digital tools that facilitate the delivery of appropriate care virtually;
- Utilization of centers of excellence that, even when considering travel costs, are often justified due to cost and outcome deltas;
- Smarter analytics and more automated care-coordination services that surface more efficient sites of service to providers (and patients);
- Provider quality transparency services that evaluate the efficacy of a given provider, thereby putting their cost in context;
- Study after study shows there is minimal association between the cost of services and the outcome;
- Patients often use brand names or reputability as heuristics of quality, but this is often inaccurate, particularly on a service-by-service basis (see: Gawande);
- Patient education support, which is critical for trust-building and care-routing, and important to health equity, patient compliance with care plans, and the improvement of overall health.
Prevention and Preemption:
Proactive Management vs. Reactive Triage
As the proverb goes: “a stitch in time saves nine.” While it has become tautological in discussions around value-based care, impactful preventive medicine is the ultimate lever to improve outcomes and sustainably reduce costs. It has demonstrable impact on reducing costly hospital admissions; yet, it is provided unevenly to different populations, adhered to unevenly by disparate cohorts of patients, and most organizations that ‘move toward value’ fail to effectively mobilize around investments in preventative care that sufficiently address these issues.
We believe that this dearth of progress has three main causes:
- Enduring misalignment of core economic drivers
Time after time, we see organizations take incremental steps toward value-based economic models that fail to produce the results needed to justify further investment and progression on the value-based spectrum. This approach begs the question. It is incorrect to assume that moving part of the way toward more fully realized value-based economic models will surface a proportionate reward. We find that incremental approaches are often disruptive enough to discourage more fulsome realignment, whereas full adoption of a better-aligned model may hurt less in due course. In other words: rip the bandaid off.
At Pearl, we believe that capitation is necessary to engender sufficient freedom from anachronistic care models, and total-cost-of-care risk exposure is required to align financial incentives with value creation.
- Unhelpfully broad preventive-care protocols
When preventive-care models recommend actions based on broad demographic swaths, care may not feel tailored to individuals, which can decrease patient trust that a given recommendation is actually best for them. Moreover, the deluge of recommendations that often accompany such engagement can inundate patients with so much information and to-dos that it can be overwhelming and lower compliance — this is often especially true for the patients who would most benefit from preventative care.
Instead, we propose that targeted interventions and recommendations, based on asymptotically-specific and comprehensive patient data, will allow providers and patients to focus on the preventive protocols most likely to provide the best ROI from patient efforts. Additional work can be done once a patient has demonstrated progress in the most critical areas, leveraging feelings of momentum that are so necessary to motivate ongoing life changes.
Further, by surfacing only the most impactful opportunities and automating appropriate follow-up interactions, we can ensure that providers have the bandwidth required to manage a patient’s longitudinal progress.
- Difficulty maintaining longitudinal contact with patients
Most provider practices are not oriented around the routine engagement that is required to ensure commitment to and compliance with preventive-care protocols. Annual checkups with minimal intra-year contact between practitioners and patients are not conducive to maintaining the ongoing behavior adjustments necessary to sustain healthier lifestyles.
Transitioning primary care to a capitated, at-risk payment model will obviate the need for ongoing engagement to take the form of burdensome office visits. Practices can instead engage patients across a variety of modalities to check in on progress and address patient issues or concerns. When paired with technology that can track patient engagement preferences, surface reminders to practice staff, and automate actions on behalf of practitioners when clinically appropriate, capitated, at-risk payment models can facilitate more consistent patient interactions that drive increased patient engagement and better outcomes.
Tactics to address likely low-hanging fruit
While this is not meant to be an exhaustive list, here we explore some of the main drivers of spend and levers/tools available to those looking to succeed in value. (H/T to Pearl’s CPO Jen Rabiner for much of the research around this.).
Avoidable (Re-)Admissions / ED Presentations
Depending on the exact population and region of the country, there are likely 150-200 avoidable Emergency Department visits per 1,000 Medicare beneficiaries on an annual basis.
Figure 1: Potentially avoidable emergency department visits among Medicare beneficiaries age 65 and older per 1,000 beneficiaries
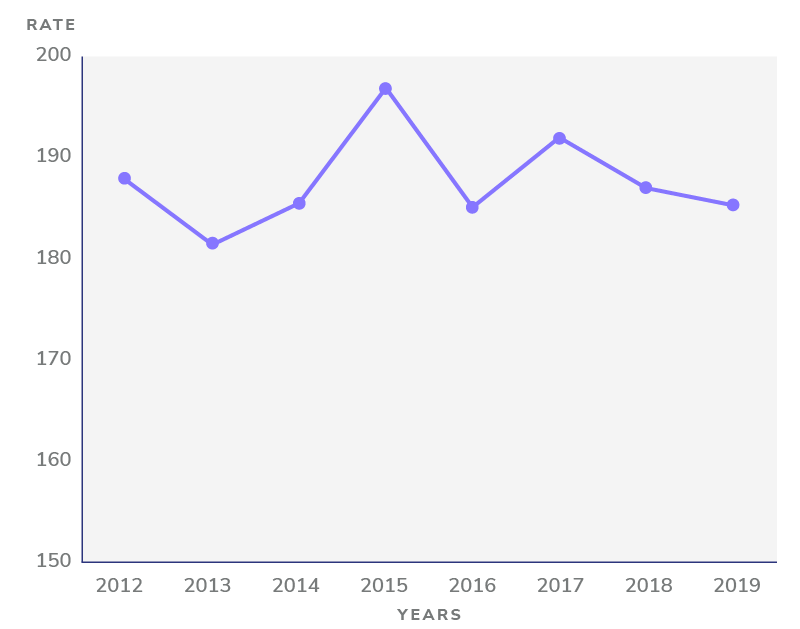
Data: Chronic Conditions Data Warehouse (CCW), via CMS Geographic Variation Public Use File; Source: The Commonwealth Fund
Figure 2: Potentially avoidable emergency department visits among Medicare beneficiaries age 65 and older per 1,000 beneficiaries, by income
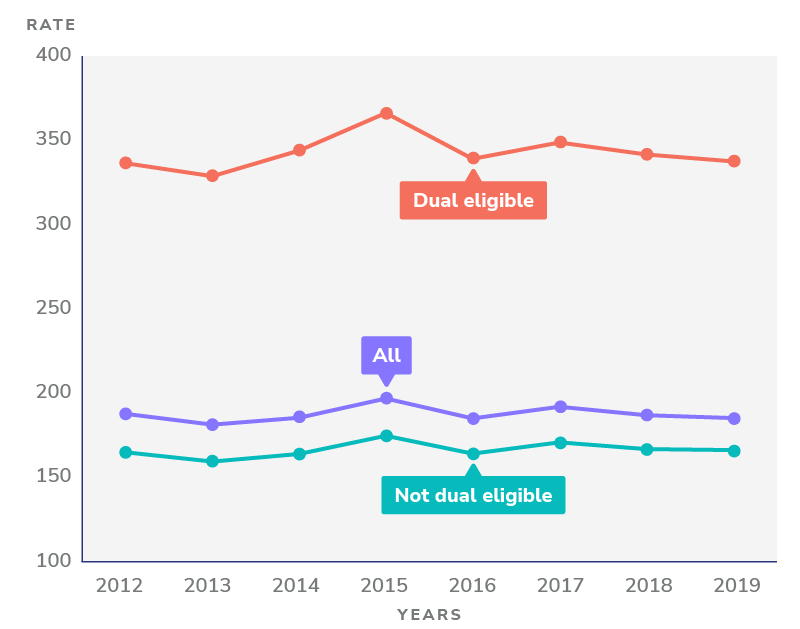
Data: Chronic Conditions Data Warehouse (CCW), via CMS Geographic Variation Public Use File; Source: The Commonwealth Fund
Notes: Vast differences between dual-eligible and not dual-eligible patients; income and the implied disparate access to preventive care inform a huge discrepancy.
Further, 30% of ED visits that take place for beneficiaries aligned to a Medicare ACO are likely avoidable. Given the high cost of ED visits and the likely result of an unnecessary hospitalization, mitigating unnecessary visits is a clear area of opportunity. For reference, the average cost of a Medicare readmission is $15,500, which is more than the average expenditure target that Medicare sets for a beneficiary for an entire year.
Figure 3: Average cost of 30-day all-cause adult hospital readmissions, by expected payer, 2018
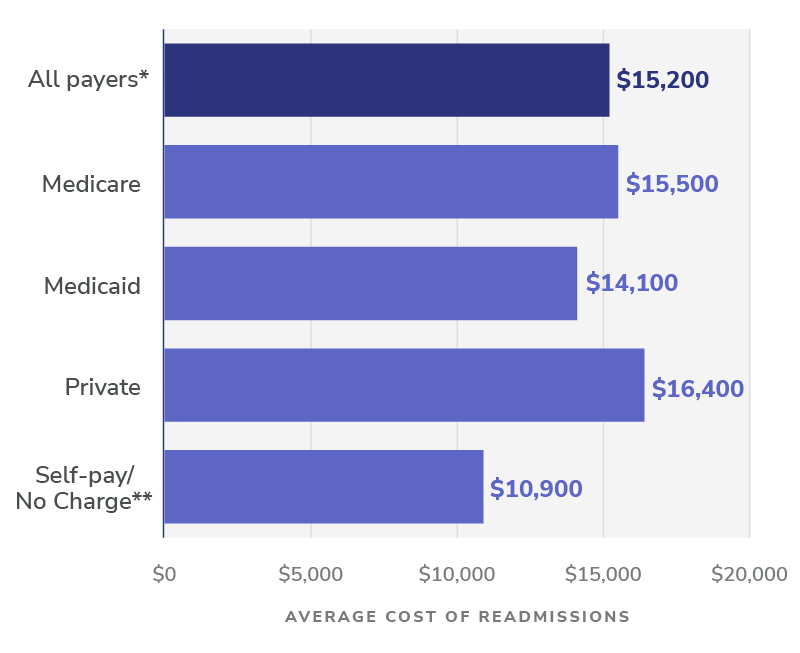
Notes: Number of readmissions is rounded to the nearest hundred. Average cost of readmission is rounded to the nearest $100. * Statistics for “all payers” include 77,900 readmissions with an expected payer of “other” or missing/invalid expected payer information. ** Self-pay/No charge: includes self-pay, no charge, charity, and no expected payment.
While having a general sense of your patients’ care patterns and risk factors is necessary to develop a perspective on appropriate preventative protocols, there are also more targeted initiatives that providers looking to manage in value should consider. These include:
- ADT alerts for patients who present at an ED or hospital to enable rapid triage;
- After-hours patient support to avoid an ED visit due to lack of clinical access;
- Home visits for high-risk patients who may otherwise forego care;
- Direct admissions to skilled nursing facilities for those who meet appropriate clinical criteria;
- Check-ins with patients within a week post-discharge.
Unnecessarily Long Stays in Post-Acute Settings
Skilled Nursing Facilities (SNFs) and similar institutions provide a valuable service in managing patients immediately following an acute event (and sometimes in lieu of hospitalization, when clinically appropriate). Indeed, SNFs are often both more clinically appropriate and more cost-effective for certain care needs than hospitals. However, SNFs are generally remunerated based on the length-of-stay of the patients in their care. PCPs who actively manage patients out of SNFs when clinically appropriate, and instead provide home health services (usually via a partner agency), will drive savings.
Avoidable Specialist Visits
While specialist care can be a critical component of managing complex or chronic patients when clinically appropriate, referrals to specialists can also add unnecessary cost, increase patient burden, and result in incomplete feedback loops to PCPs, and are driven instead by PCP burden and areas of borderline concern. Services like ‘curbside consults’, where a PCP can get a specialist’s views on a patient case in their area of expertise without a formal patient visit can reduce such unnecessary utilization.
Ensuring Accurate Benchmarks
While all of the above is about reducing wasteful utilization, value-based math also has a denominator against which costs are measured to calculate savings — in ACO REACH, it’s called a benchmark (for health plans, this is the annual premium). Benchmarks in REACH and similar models are calculated via a number of complex inputs; among them is the Risk Adjustment Factor (RAF). Unfortunately, many entities have run afoul of regulations by fraudulently inflating their RAF scores through unwarranted diagnoses and overdiagnosing. In a competitive-RAF environment like REACH (where, akin to ACA risk-adjustment methodologies, the average RAF of peers informs the baseline), it is all the more important to ensure accurate formal and annual diagnoses to avoid artificially deflated benchmarks that do not acknowledge the actual disease burden of patients (and harder journeys to achieving savings).
In Part III of our “Value-Based Care Playbook,” we continued to examine how value-based organizations can support primary care providers in managing the care journeys of their patients. In this post, we paid particular attention to the tools necessary to support longitudinal compliance with preventive measures, thereby avoiding the locality conundrum that dominates cost calculus in too many U.S. healthcare markets. As Pearl continues to empower primary care providers in value-based care models, we will continue to share lessons learned in future installments.