Value-based care has been part of our healthcare lexicon for the last 15 years when, in 2006, Michael Porter and Elizabeth Olmsted Teisberg are credited with introducing this phrase in their book Redefining Health Care.
The basic premise: organize our healthcare system in a way that compensates the provider of care for delivering value to their patients.

A Brief History
It’s no secret that healthcare spending in the United States has been climbing higher each year, and that both public and private payers have been looking for ways to slow down this growth. Throughout the course of modern US healthcare, we have struggled to create a fair and efficient reimbursement scheme that aligns the incentives of patients, providers and payers. Prior efforts to contain these costs — most notably, the rise (and downfall) of managed care in the 1990s — kept the focus on managing financial risk and reducing costs.2 The concepts of clinical quality or patient satisfaction, both current measures of “value”, were not part of the equation until the onset of value-based care (VBC).
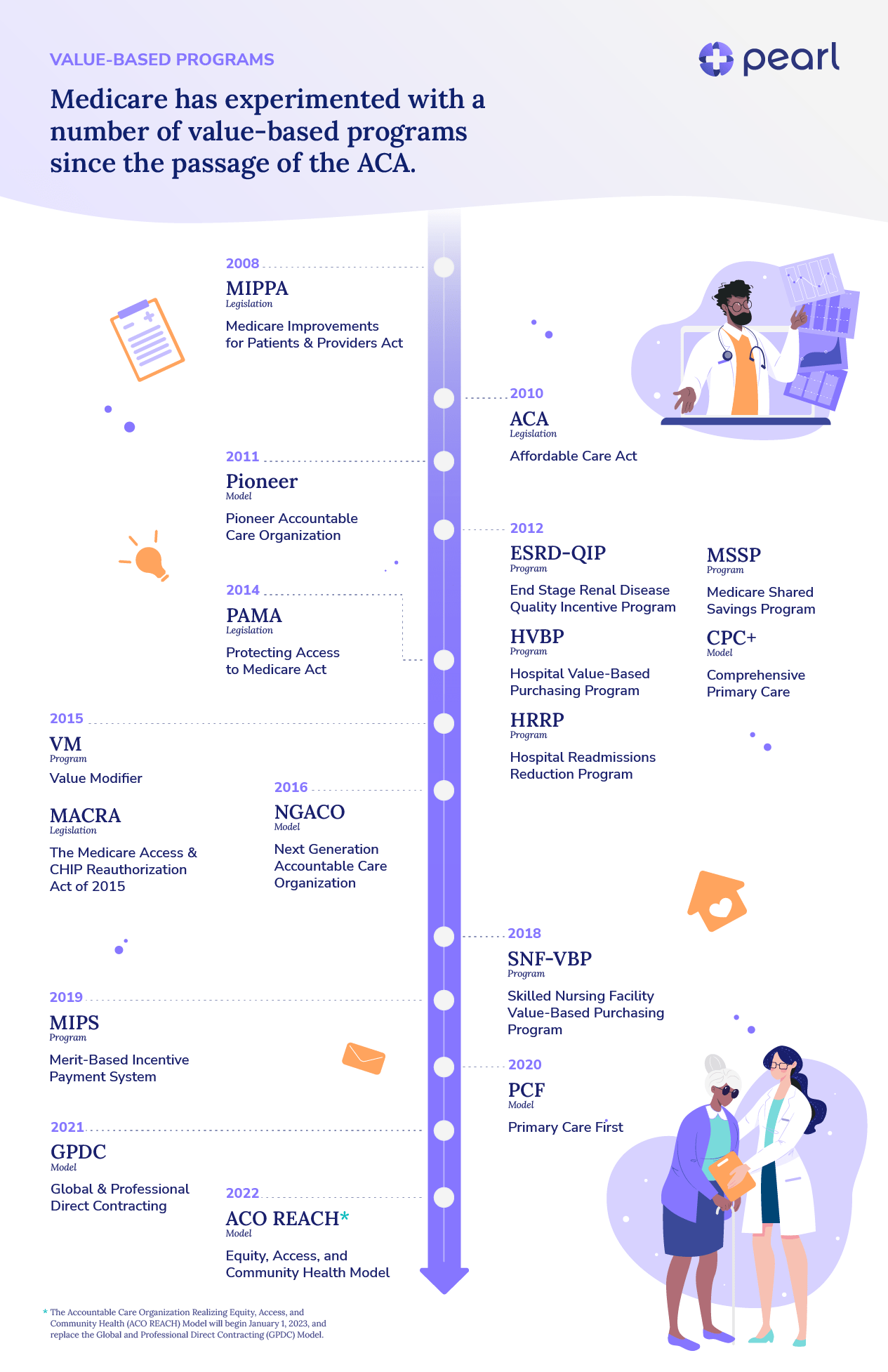
Costs continued to rise in the 2000s, due largely to regional market share dominance, the deployment and over-utilization of advanced procedures, the increasing sub-specialization of providers and the lack of appropriate checks on medication costs. As a result, VBC programs sponsored by both commercial and government insurers arose. The initiatives implemented by the Centers for Medicare and Medicaid Services (CMS) go back to 2005, when 10 providers enlisted in the Physician Group Practice Demonstration,3 and 2008, when the Medicare Improvements for Patients and Providers (MIPPA) established the End-Stage Renal Disease Quality Incentive Program (ESRD-QIP) (implemented starting in 2012).4 This program was the first of its kind from CMS, wherein payment was linked to quality measures.5
In the following year, Blue Cross Blue Shield of Massachusetts implemented its Alternative Quality Contract (AQC).6 The AQC gives providers a ‘global budget’ to manage the overall spend on their patients, and includes both clinical quality and patient satisfaction. Eight years into the program, a New England Journal of Medicine study shows a 12% slow in spending under this contract.7
As the first decade of the twenty-first century came to a close, the Affordable Care Act (ACA) was passed in 2010. VBC programs grew in both size and scope following the passing of this historical piece of legislation. Notably, the ACA established the Center for Medicare and Medicaid Innovation (CMMI) to design and test new VBC programs.
Of the over 40 programs implemented by CMMI,8 one of the biggest programs has been the Accountable Care Organization (ACO). Similar to the AQC contract, ACOs incentivize providers to reduce overall spending while also meeting certain clinical quality and patient satisfaction measures. Since their initial implementation, CMS has implemented multiple ACO models.9 Commercial payers have followed suit, implementing ACO-like models for their patient populations.10
In 2015, Congress passed the Medicare Access and CHIP Reauthorization Act (MACRA) to further accelerate the adoption of VBC. This legislation created the Merit Based Incentive Payments System (MIPS) to streamline multiple quality-related programs, as well as incentivized physicians to participate in Alternative Payment Models (APMs).11
What’s Next?
So, after all of this legislation and a veritable alphabet soup of program acronyms — has VBC achieved its multi-pronged mission of achieving cost savings by providing value to patients? There is no clear consensus, and results are mixed.12, 13 However, even if the models and mechanisms are evolving, it’s clear that VBC as a strategy isn’t going anywhere. New programs that build upon the lessons of prior successes and failures are now being implemented by CMMI, like Primary Care First (PCF) and ACO REACH (redesigned from Direct Contracting).14, 15Pearl Health’s Role in VBC
At Pearl Health, we believe in the promise of VBC. We also know that evolution and iteration that build upon past successes and learnings are necessary. We are industry experts who have worked in all corners of healthcare, and we’ve come together to build Pearl because we believe in the future of VBC — one where we control costs through aligned incentives that maintain a high quality of care and a positive experience for providers and patients alike.
In particular, we are excited about the potential of the ACO REACH Model. We believe that continuing to put primary care at the forefront of patient care is the right thing for patients. We also believe that patients will benefit from primary care physicians who have more autonomy and flexibility than they experience in the predominantly volume-based paradigm in which they exist today.
While we believe in the potential of VBC, we also know that these programs are complex for all stakeholders involved to navigate. A core part of our mission is to make VBC programs more accessible, to ensure maximum participation and maximum success.
The technology and services we are building out today are focused on exactly these beliefs — moving primary care physicians into care and payment models that allow them to practice medicine with autonomy and flexibility, and helping them succeed clinically and financially when they get there.
How much more could your practice earn with Pearl?
- Michael E. Porter and Elizabeth O. Teisberg, Redefining Health Care: Creating Value-Based Competition on Results. Boston, Mass: Harvard Business School Press. 2006.
- Stanford GSB Staff, “Managed Care: What Went Wrong? Can It Be Fixed?,” Stanford Graduate School of Business, November 1999.
- “Medicare Physician Group Practice Demonstration,” CMS Innovation Center, May 2021.
- Daniel Weiner and Suzanne Watnick, “The ESRD Quality Incentive Program-Can We Bridge the Chasm?,” American Society of Nephrology, June 2017.
- “ESRD Quality Incentive Program,” CMS, March 2022.
- “Alternative Quality Contract AQC,” Blue Cross Blue Shield of Massachusetts, April 2021.
- Zirui Song et al., “Health Care Spending, Utilization, and Quality 8 Years into Global Payment,” New England Journal of Medicine, July 2019.
- “‘What is CMMI?’ and 11 Other Faqs about the CMS Innovation Center,” Kaiser Family Foundation, February 2018.
- “Accountable Care Organizations (ACOs): General Information,” CMS, July 2022.
- “Our Take: Commercial ACOs top 3,000 agreements, 30 million members,” Darwin Research Group, August 2019.
- “MACRA, MIPS, and APMs,” CMS, April 2022.
- Todd Shryock, “Does Value-Based Pay Have a Future?,” Medical Economics Journal, September 2019.
- Kevin Hutchinson, “Is Value-Based Care Stalled?,” Gibson Consultants, October 2020.
- “Primary Care First Model Options: CMS Innovation Center,” CMS Innovation Center, August 2022.
- “Exploring the Direct Contracting Model: A Revolution in Healthcare,” Pearl Health, May 2021.


