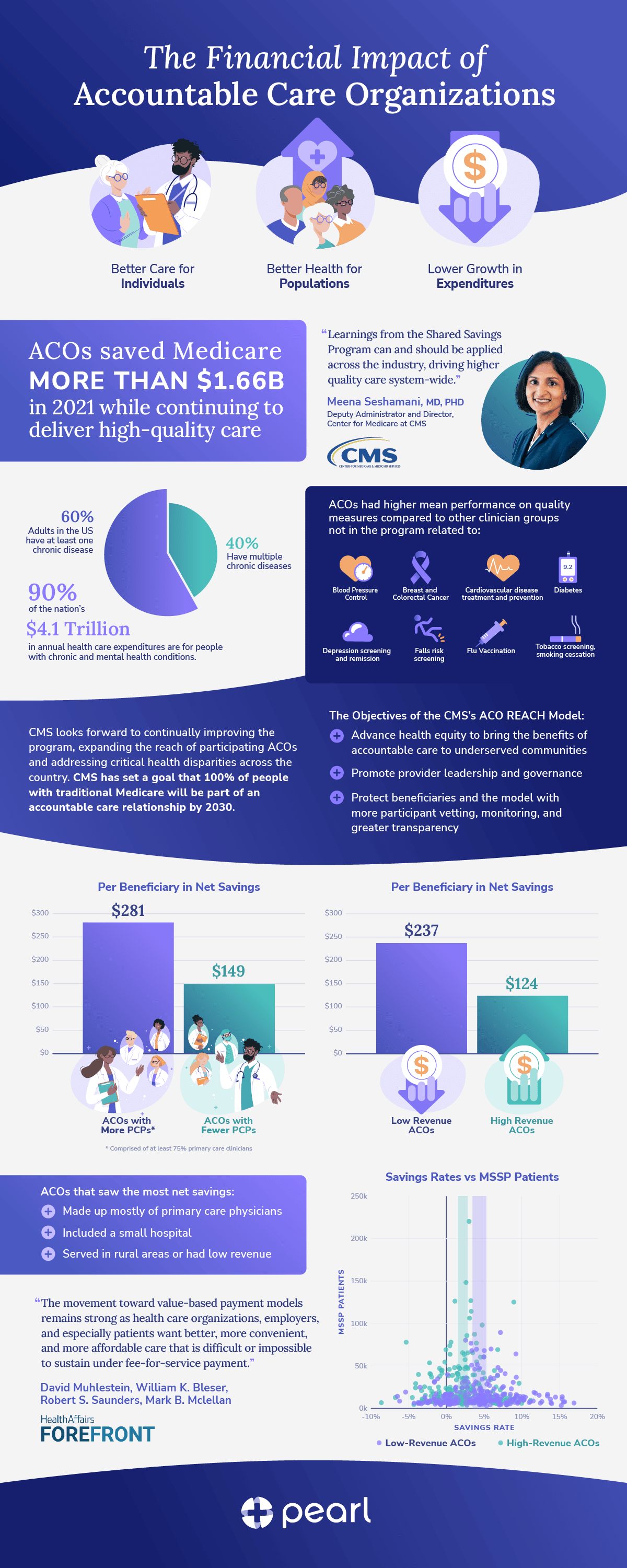
The Centers for Medicare & Medicaid Services (CMS) announced that Accountable Care Organizations (ACOs) in the Medicare Shared Savings Program saved Medicare — and US taxpayers — $1.66 billion in Performance Year 2021 compared to spending targets. This marks the fifth consecutive year that the program has generated overall savings while continuing to deliver high-quality patient care.1
In 2021, ACOs had higher mean performance on quality measures compared to other clinician groups not in the program, and 99% met the quality standard required to share in savings. This includes higher performance for quality measures related to:

Based on the success of the Medicare Shared Savings Program, the mission to continually improve the quality of care for people with Medicare, and the enormous opportunity to generate savings and create value in our healthcare system, CMS has set a goal that 100% of people with traditional Medicare will be part of an accountable care relationship by 2030.5
There’s more value within REACH
In addition to proposing ways to further expand these innovative Medicare ACOs, CMS created the ACO REACH model in 2022. ACO Realizing Equity, Access, and Community Health (ACO REACH) was designed to increase access to value-based care models, to innovate and inform both current and future ACO models, and to advance health equity and access to care for all patients, especially those in underserved communities.
The Objectives of the ACO REACH Model:
- Advance health equity to bring the benefits of accountable care to underserved communities
- Promote provider leadership and governance
- Protect beneficiaries and the model with more participant vetting, monitoring, and greater transparency
As we explain in the sections that follow, the model’s emphases on increasing access to value-based care, ensuring that ACOs are predominantly led by PCPs, and strengthening the participant vetting process are well supported by the Medicare Shared Savings performance data from 2021. As such, we believe that this data suggests that many of the policies enacted in ACO REACH will lead to strong performance and increased economic returns over time.
Increasing access to underserved communities
It has long been the case that ACOs have been concentrated around urban areas of the country, and that many rural regions still do not have significant ACO presence.6 Because of this, ACO REACH was specifically designed to address the stark regional and socioeconomic disparities in access to value-based models.
The results from the Medicare Shared Savings Program in 2021 show that “the type of ACOs that saw more net savings tended to be low-revenue, meaning they were mainly made up of physicians, included a small hospital, or served in rural areas.” 7 These results are consistent with previous findings,8, 9, 10 and serve as yet another reason to believe that the expanded access to value-based care models through the REACH program is likely to result in even more savings for Medicare, more revenue for PCPs, and, most importantly, more holistic care for people with Medicare.
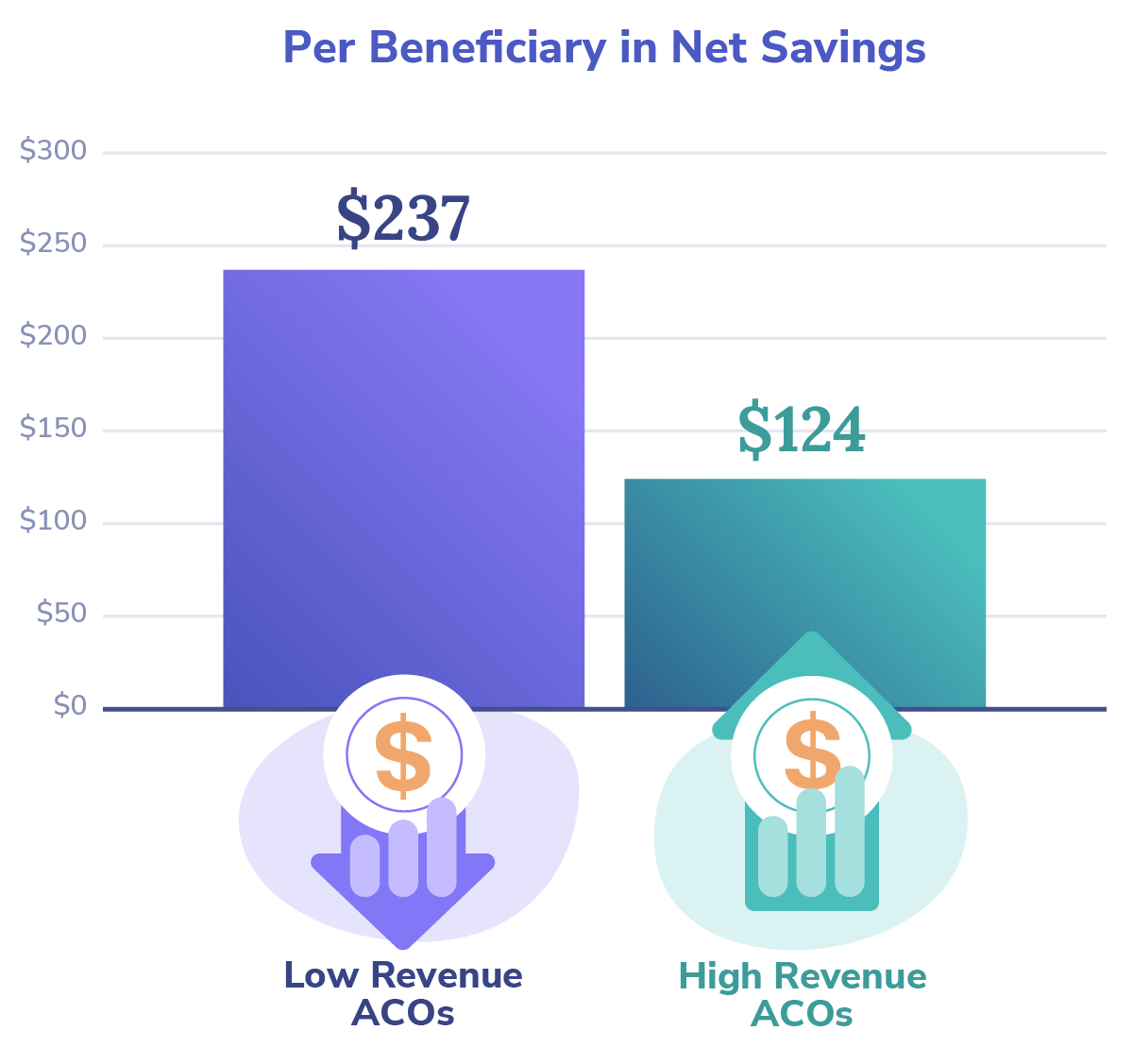
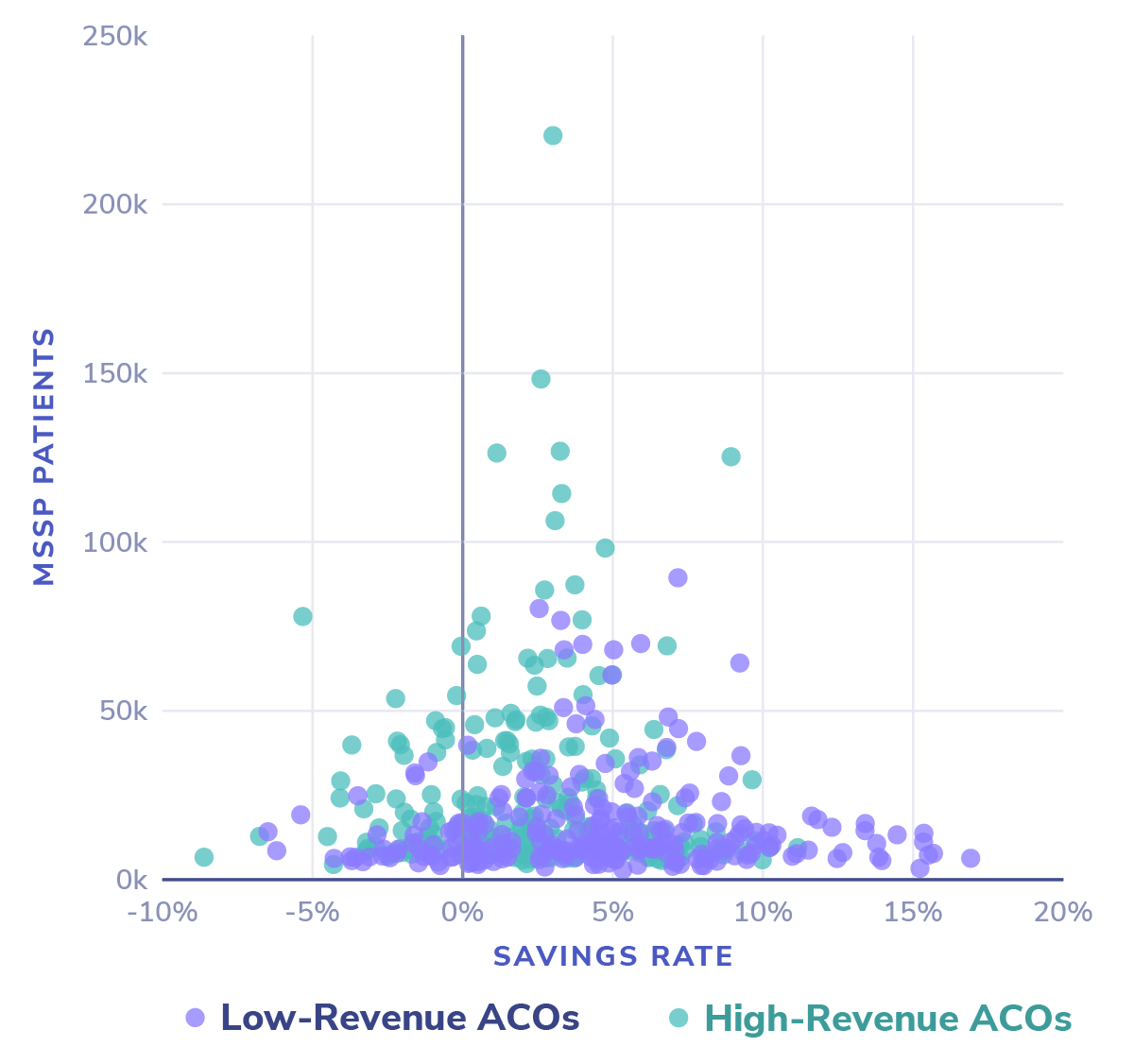
For more detail, the scatterplot graph below shows each MSSP with the number of aligned lives on the Y-axis and the percent savings or losses on the X-axis. As is apparent with the purple dots, the overwhelming majority of MSSPs generating the highest percent savings are the low-revenue ACOs. These smaller, physician-led, and potentially rural ACOs are ideal candidates for REACH, as REACH rewards ACOs for increasing the health equity of underserved populations via an upward benchmark adjustment and allows for the sharing of up to 100% in the savings generated.
Advancing the transition to provider-led risk
Beyond its critical mission to advance health equity, ACO REACH was also designed to address feedback from stakeholders in previous value-based care models.12 The focused engagement with PCPs via newly-increased governing board participation requirements and the newly-introduced primary care capitation concept demonstrates CMS’ willingness to partner with the patients’ primary caregivers and help reward them for their tireless efforts.
The 2021 MSSP performance data supports the PCP governance mandates in REACH, showing that ACOs comprised of at least 75% primary care clinicians provided materially higher net savings than ACOs with fewer PCPs, in fact, 88% higher on average:
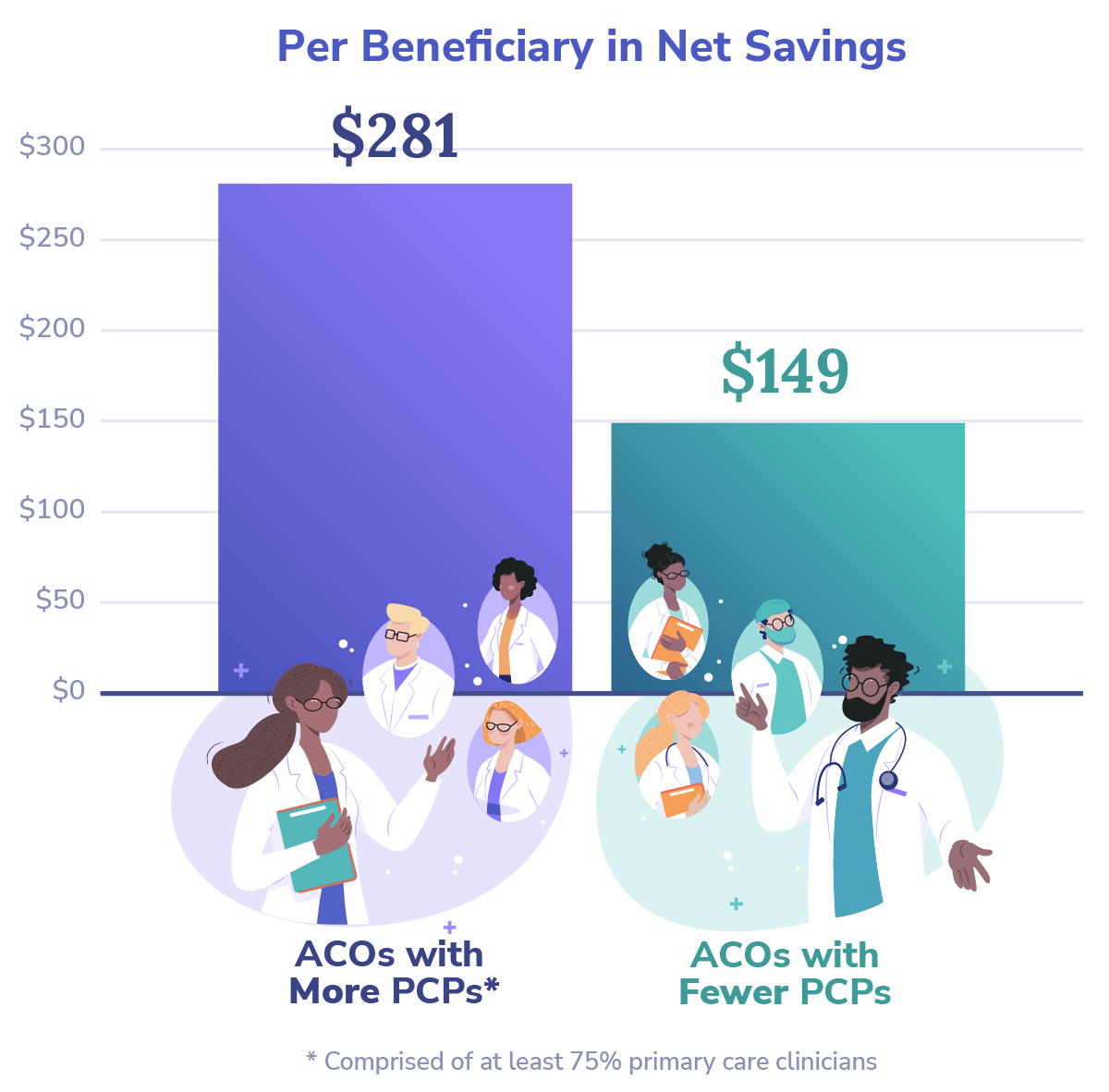
These results affirm the importance of primary care in the successful implementation of value-based care models and offer proof for the fortuitousness of the ACO REACH model in its stipulation that: ”At least 75% control of each ACO’s governing body generally must be held by participating providers or their designated representatives.” 13
Before approving REACH ACOs for 2023 participation, CMS requested additional information on the ACOs’ “ownership, leadership, and governing board to gain better visibility into ownership interests and affiliations to ensure participants’ interests align with CMS’ vision.” 14 REACH ACOs not only go through a more rigorous up-front screening process, but are also subject to “robust monitoring of participants, and transparency into the model’s progress through implementation.” 15
In combination, we believe that these changes will increase adherence to the practices that underpin value-based care, and will reward patients with higher quality sustained care as participating providers — and the model itself — become more successful over time.
Aligning financial incentives with value creation
There is no doubt that all Medicare ACO stakeholders should be indebted to CMS and the Medicare Shared Savings Program as one of the most successful programs to come out of the Affordable Care Act. However, while it has greatly advanced patient care and offered tremendous learnings (through both successes and shortcomings), we believe that it often shifts priorities too slowly to rise to the emergent challenges and opportunities in our ever-evolving healthcare ecosystem.
At Pearl Health, we believe that one of its greatest inhibitors to true progress is the enduring misalignment of core economic drivers. In our view, our healthcare system cannot realize the full promise of value-based care until a preponderance of providers transition away from the often perverse incentives associated with fee-for-service payments and put more ownership, or risk, on the providers.
Read More: Tactics for Succeeding in Value-Based Care
One mechanism through which ACO REACH promotes health equity and focuses on bringing the benefits of accountable care to underserved communities is an “innovative payment approach to better support care delivery and coordination for patients” in these communities.16

David Muhlestein, William K. Bleser, Robert S. Saunders, Mark B. Mclellan
In REACH, primary care providers can begin the transition away from fee-for-service (FFS) in a revenue-neutral way — by moving from volume-based FFS payments for the number of primary care services they provide to stable, monthly capitation payments for revenue CMS estimates a provider would otherwise make from a given patient panel. Transitioning from FFS better positions PCPs to align financial incentives with patient care (capitation), creates incentives to ensure that vulnerable beneficiaries do not slip through the cracks that often appear during otherwise non-reimbursable moments (quality measures), and provides opportunities for PCPs to generate additional revenue for keeping patients healthy (shared savings).
Read More: Improving Primary Care Providers’ Prospects
At Pearl Health, we’re heartened by the 2021 savings and performance results from the Medicare Shared Savings Program and energized by the potential implications for ACO REACH. We’re proud to be building technology to enable the next generation of providers and accountable care organizations to succeed in this model and help our system transition from volume to value.
- CMS, Press Release, “Medicare Shared Savings Program Saves Medicare More Than $1.6 Billion in 2021 and Continues to Deliver High-quality Care,” August 30, 2022.
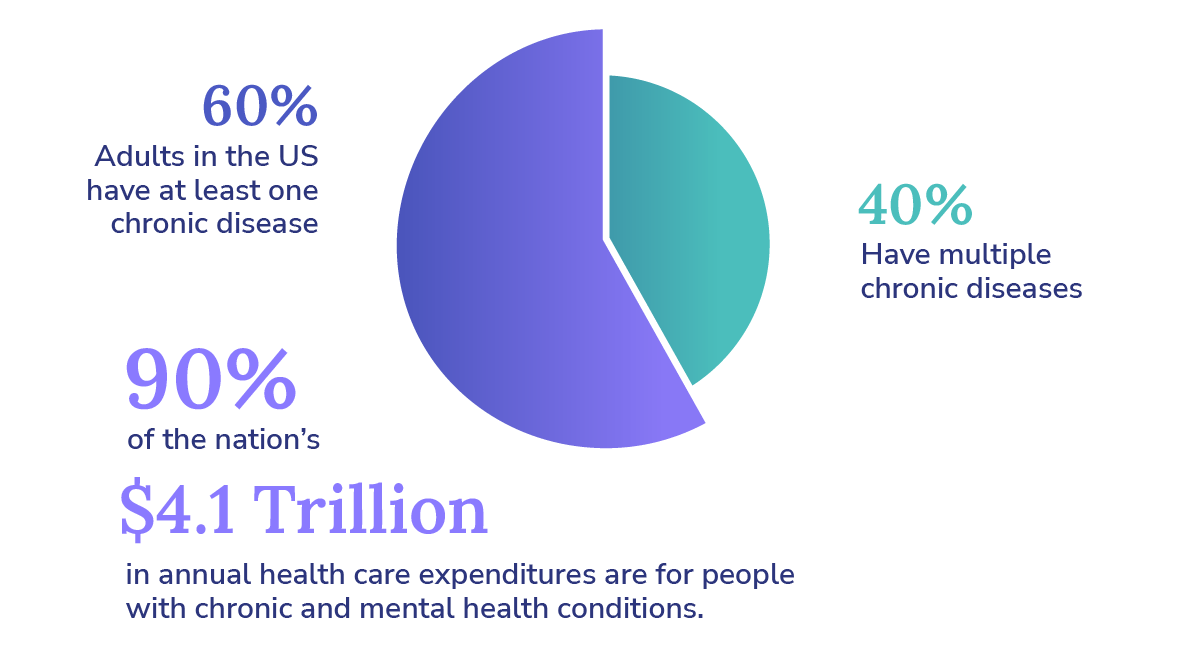
- CDC, National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP), “Chronic Diseases in America,” May 6, 2022.
- CDC, National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP), “Health and Economic Costs of Chronic Diseases,” September 8, 2022.
- CMS, Press Release, August 30, 2022.
- CMS, Press Release, August 30, 2022.
- David Muhlestein, et al., “All-Payer Spread of ACOs and Value-Based Payment Models In 2021: The Crossroads and Future of Value-Based Care,” Health Affairs Forefront. June 17, 2021.
- CMS, Press Release, August 30, 2022.
- Kyle Gibler, et al., “Physician Employment: The Path Forward in the COVID-19 Era,” McKinsey & Company. July 17, 2020.
- Lawrence Casalino, et al. “Small Primary Care Physician Practices Have Low Rates of Preventable Hospital Admissions,” Health Affairs (Project Hope). U.S. National Library of Medicine, September 2014.
- Lawrence Casalino, et al. “Medical Group Characteristics and the Cost and Quality of Care for Medicare Beneficiaries,” Health Research and Education Trust. U.S. National Library of Medicine, December 2018.
- CMS, Press Release, August 30, 2022.
- CMS, Innovation Models, “ACO REACH,” Centers for Medicare & Medicaid Services, August 25, 2022.
- CMS, Innovation Models, August 25, 2022.
- CMS, Innovation Models, August 25, 2022.
- CMS, Innovation Models, August 25, 2022.
- CMS, Innovation Models, August 25, 2022.
- Muhlestein, Health Affairs Forefront, June 17, 2021.
.