When patients are discharged from the hospital to their home, they become responsible for managing their condition and coordinating additional care. They often need to fill new medications and schedule follow-up appointments with primary care providers (PCPs) or specialists. Patients receiving complicated or unclear discharge instructions may not fully understand what’s required of them, which can lead to adverse events and unplanned hospital readmissions. Additionally, critical information following these hospital stays is often not sent to PCPs who manage their patients on a day-to-day basis.
One study found that in 2003, 19.6% of Medicare patients who were discharged from a hospital were readmitted to a hospital within 30 days.1 The study goes on to estimate that the cost to Medicare of these unplanned rehospitalizations was $17.4 billion. While readmission rates have since decreased (from 21.5% in 2007 to 17.8% in 2015 for targeted conditions and from 15.3% to 13.1% for non-targeted) and some readmissions are unavoidable due to disease progression,2 it’s clear that this remains a significant issue in our healthcare system. It’s also clear that preventing avoidable readmissions can improve the quality of life for patients while also reducing overall healthcare costs.
The best way to prevent avoidable hospital readmission is to place PCPs at the center of care coordination.
At Pearl, we believe the best way to prevent avoidable hospital readmission is to place PCPs at the center of care coordination across specialties, serving as the hub for post-discharge patient care. With PCPs empowered to investigate and identify which patients are at risk, they are naturally better equipped to help develop strategies to prevent readmission.
However, many practices are not notified when their patients are admitted or discharged from the hospital or emergency department. Because they don’t have this information, they aren’t able to schedule follow up appointments to ensure their patients are set up for success. This missing clinical information is one of the biggest barriers to PCPs in improving patient care.
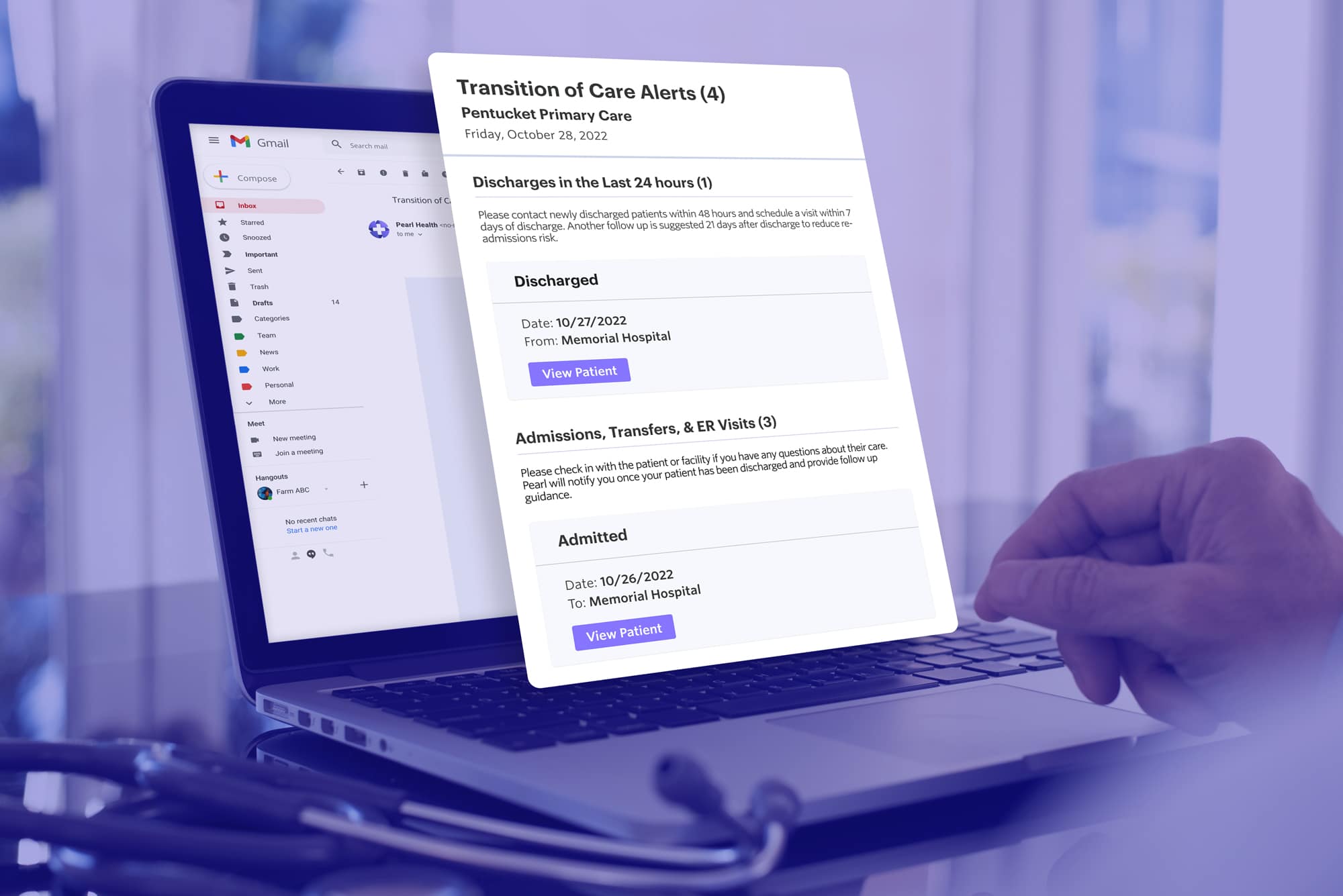
To enable PCPs to act as the hub for post-discharge patient care and remedy this paucity of information, we developed an integration that streams admit, discharge, and transfer (ADT) data directly into the Pearl Platform. It provides practices with real-time updates whenever patients experience acute or post-acute care events, including detailed information about the event so clinicians can seamlessly coordinate medical care.
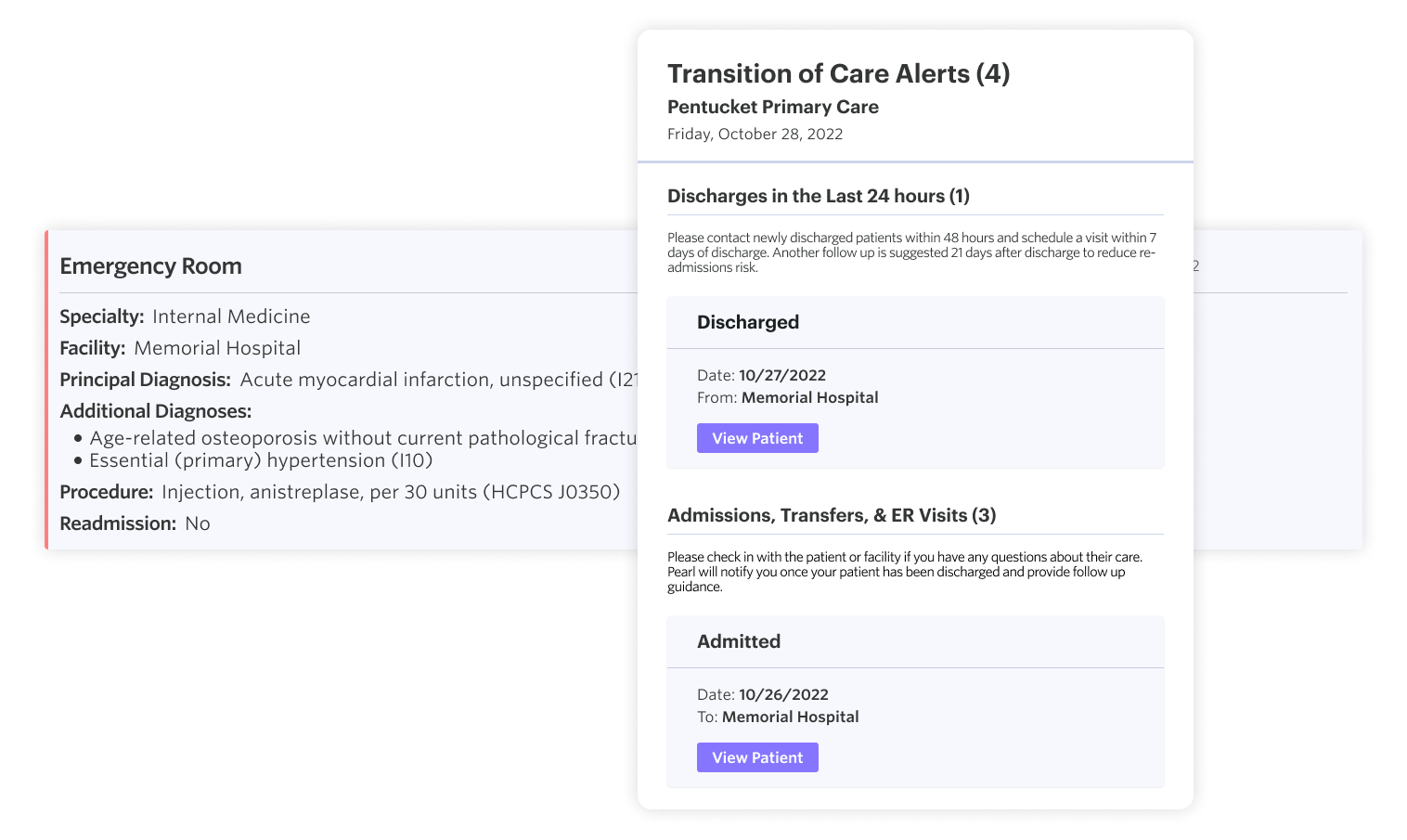
By improving visibility into hospitalizations, practice staff can better monitor patients under their care, ensure proper post-discharge behaviors, and schedule follow-up office visits as needed. This improves care while also helping to satisfy the Timely Follow Up and All Cause Readmissions (ACR) Quality Measures in Medicare’s ACO REACH model.
Pearl’s ADT integration is our latest step towards our goal of improving care and driving performance through data-driven insights. As we build out our capabilities, we’re focusing on workflows that target the needs of specific populations and adding more specific product features related to REACH’s timely follow-up targets.
To learn more about how we make product choices and where we’re investing next, read this blog by our Chief Product Officer, Jennifer Rabiner, on Pearl’s Product Principles.
- Stephen F. Jencks, M.D., M.P.H., Mark V. Williams, M.D., and Eric A. Coleman, “Rehospitalizations among Patients in the Medicare Fee-for-Service Program,” The New England Journal of Medicine. April 2, 2009.
- Rachael B. Zuckerman, Steven H. Sheingold, E. John Orav, et al, “Readmissions, Observation, and the Hospital Readmissions Reduction Program,” The New England Journal of Medicine. April 21, 2016.