Reflections & Renewal
As we dive into 2025, let us consider the promise the new year offers for renewal and a fresh start. Similarly, the oyster plays a vital role in refreshing aquatic ecosystems, filtering impurities, cleansing, and clarifying the waters around it. On exceptionally rare occasions, through this process of filtration and purification, the oyster may sequester debris that it eventually transforms into a pearl, turning a common impurity into a rare, valuable, and secret asset.
At Pearl Health, it’s our mission to help primary care organizations clarify the murky waters of our complex and evolving healthcare ecosystem, share insights that help physicians deliver more proactive patient care, and align payments and incentives with patient outcomes — uncovering powerful “clinical pearls” and unlocking otherwise obscured value across the system.
We’re proud of our progress on this mission, including doubling our network for the second year in a row, forming strategic partnerships with health systems and physician groups large and small, and improving our systematic approach to reducing medical costs and improving patient outcomes.
As we renew our efforts to drive this mission forward in 2025, we also reflect on our learnings along the way and celebrate the progress we have made. Below are some key moments from 2024 that leave us feeling clear, refreshed, and optimistic about the value waiting to be discovered and unlocked in 2025.
#1 From Signal to Action:
Accelerating Performance in Value
We introduced clinical signals in the Pearl Platform in 2022 and 2023 to help providers deliver better, more proactive care and improve value-based care performance—including AI-driven alerts to predict and prevent emergency department visits, reduce unplanned admissions, identify opportunities for transitional care management, and help patients with advance care planning.
In 2024, we continued to invest in our patient-centric enablement technology and incorporate new approaches to accelerate the value healthcare leaders, providers, and clinical staff are driving. We introduced new clinical signals to enable providers to more effectively help patients with Chronic Care Management and identify those who would benefit from the new dementia care program, Guiding an Improved Dementia Experience (GUIDE), released by the Centers for Medicare and Medicaid Services (CMS).
In keeping with our design principles of simplicity and ease-of-use, all of these patient insights are incorporated into a single, increasingly advanced Signal-Action Framework.
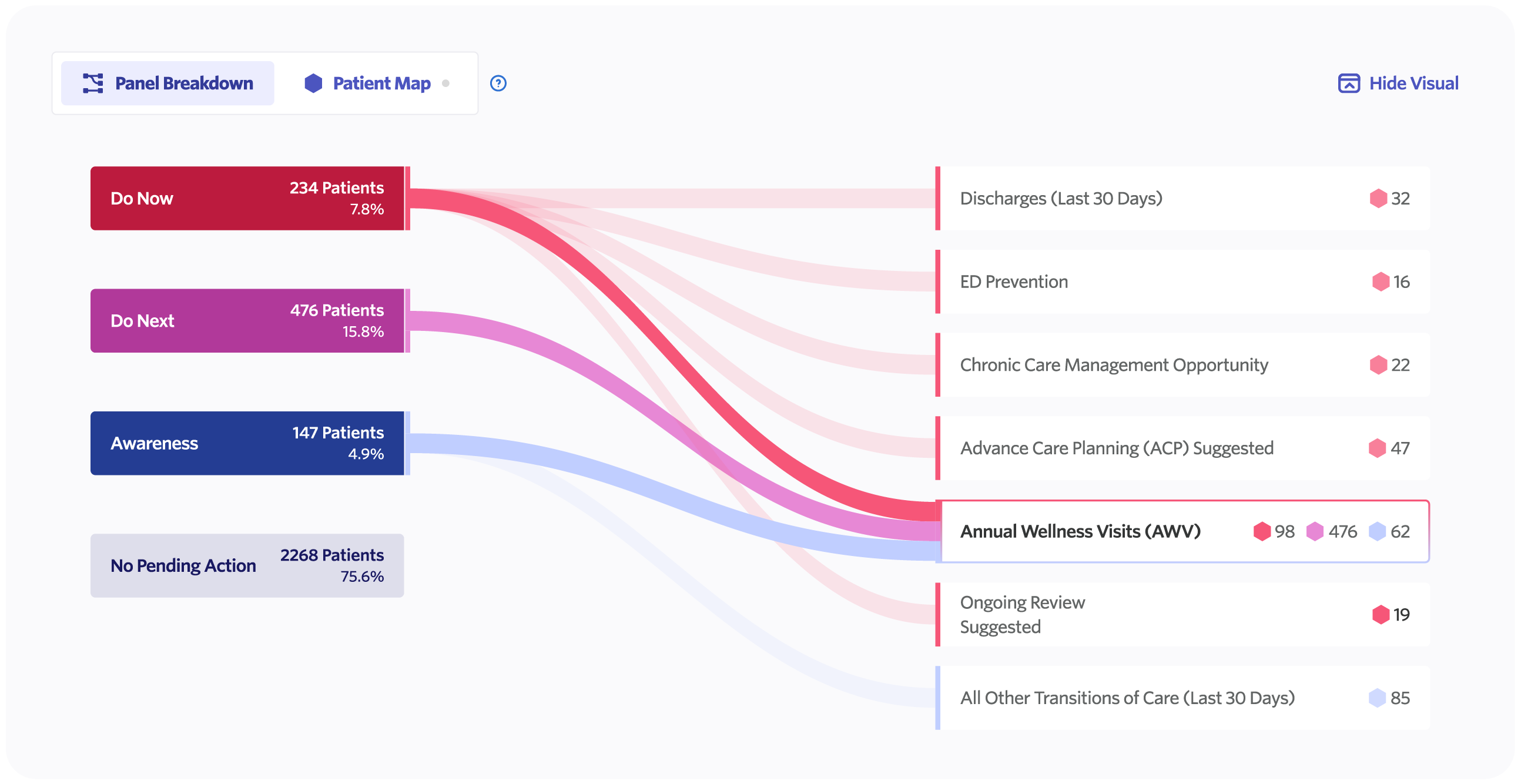
We also streamlined our panel overview and alert types, creating a new Panel Breakdown to give providers a birds-eye view of their patient panel and more easily take action for the patients most likely to benefit from proactive care.
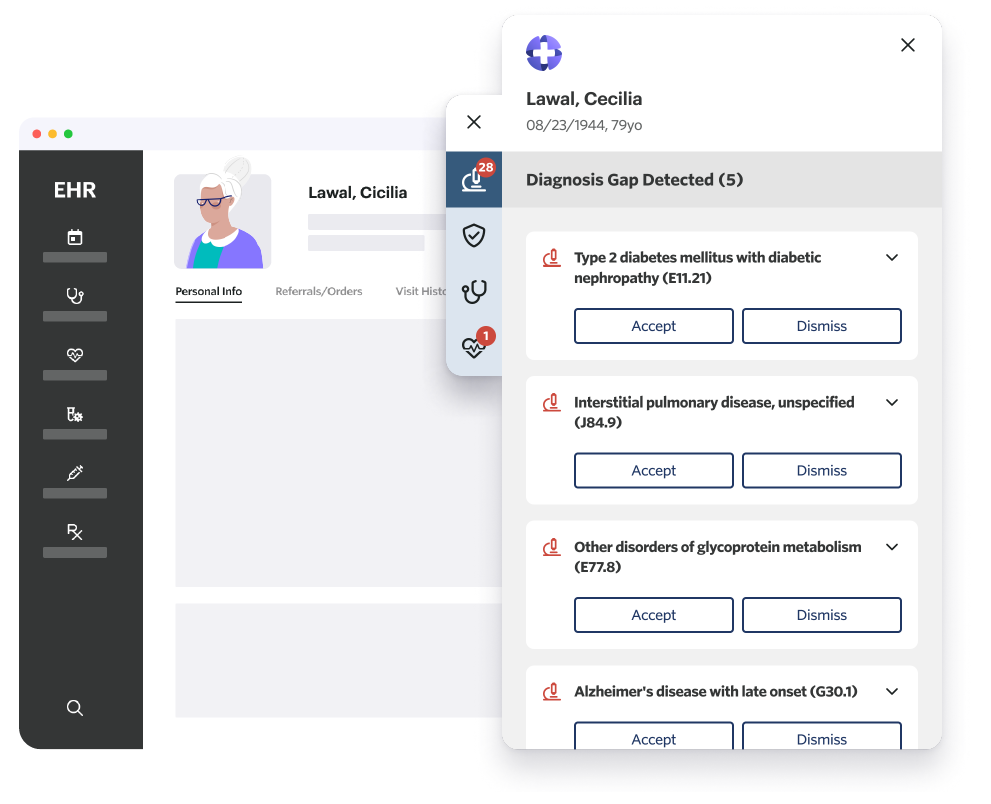
To bring insights from the Pearl Platform to providers at the point of care, we partnered with Vim to bring our Conditions to Review feature directly into the EHR experience, helping to streamline point-of-care workflows and enabling providers to spend more time focusing on the patient—instead of the computer.
Finally, we also piloted a new patient texting program to help providers schedule Annual Wellness Visits and post-discharge follow-up visits, reducing administrative burden.
At the close of 2024, we’re proud to report that since the launch of the Pearl Platform in 2022, PCPs and clinical staff have taken more than 160,000 actions through our technology—each facilitating proactive outreach and intervention for the patients who need it most, resulting in better, more efficient care that saves lives and improves the quality of life for seniors and other Medicare Beneficiaries.
This proactive outreach driven by Pearl Platform insights has had a meaningful impact on both patient care and performance in value-based care programs across our network. In 2024, providers in the Pearl Community have scheduled approximately 24,000 annual wellness visits and more than 5,000 post-discharge visits based on Pearl’s clinical signals.
Anonymized Patient Stories

-
Avoiding Unplanned Admissions for
Multiple Chronic Conditions - A patient with several chronic conditions, including congestive heart failure, type 2 diabetes, obesity, and tobacco dependence, was flagged by Pearl’s predictive algorithm as potentially at high-risk for an unplanned admission and eligible for Chronic Care Management support.
- The nurse at the patient’s primary care practice reached out to schedule an appointment. The patient’s PCP then completed a home visit to discuss risk factors and schedule an AWV to create a cross-functional care plan, improving the patient’s chronic condition management and strengthening the patient-PCP relationship.
- Avoiding Preventable Emergency Department (ED) Visits
- PCPs can play a vital role in preventing ED visits due to the deterioration of poorly-managed chronic conditions. Pearl flagged a patient who had more than 20 ED visits over a two year period, many of which were potentially preventable, as having an increased risk for preventable ED visits. Their PCP developed an escalation plan, with ongoing chronic care management, reducing the patient’s ED visits by 67% and improving the PCP-patient relationship.
As we look to 2025, we’ll continue to evolve the Pearl Platform in accordance with our product principles, leveraging the power of automation, machine learning, and generative AI to deliver patient insights throughout the care journey.
#2 Nationwide Growth:
Strengthening & Diversifying Our Network
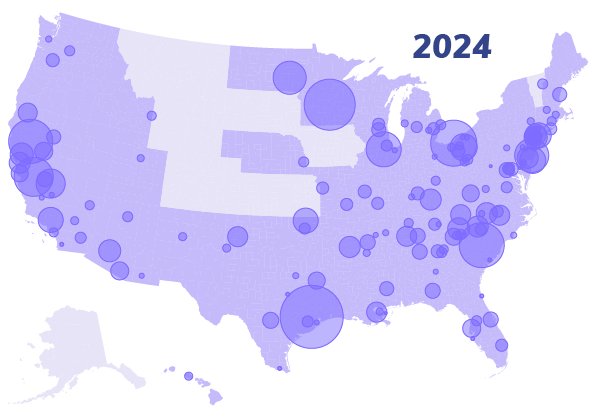
In 2024, more than 3,500 primary care providers across the US partnered with Pearl Health, roughly doubling our network for the second year running, representing more than 40× growth in three years, and expanding our network to 40+ states.
Over the past year, as our network has grown, we have also collaborated with a broader range of primary care organizations than ever before. These include health systems, physician networks, and accountable care organizations (ACOs), as well as large group practices and small private practices. This diversity underscores our commitment to fostering innovation in value-based care throughout our healthcare system.
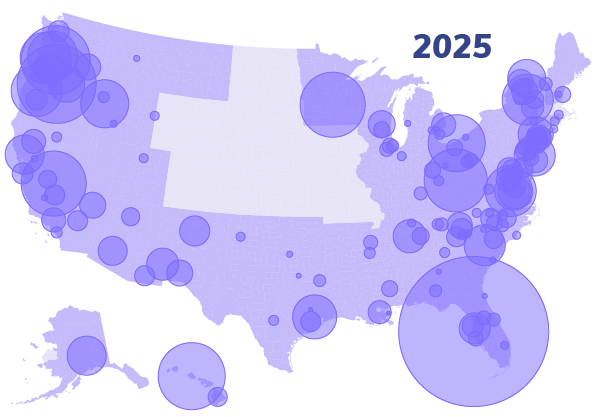
The continued growth and diversification of the Pearl Community also highlights the increasing interest among primary care organizations in adopting value-based care models. These programs shift the focus from traditional volume-driven, fee-for-service payment structures to value-based systems designed to reward better health outcomes. At Pearl, we’re dedicated to supporting this transformation by equipping our partners with the tools and strategies needed to deliver exceptional care while aligning financial incentives with patient well-being.
We’re thrilled to welcome these new partners to the Pearl Community. Together, we’re developing care models that prioritize both the patient and provider experience, enabling organizations to focus on delivering high-quality, compassionate care. As our network expands, so does our impact, and we’re excited to play a key role in shaping the future of healthcare by empowering primary care organizations to achieve sustainable, value-driven success.
#3 New Horizons:
Expanding Across Medicare Models
The Centers for Medicare and Medicaid Services (CMS)—the largest healthcare payer in the US—has set a goal to have all patients with Traditional Medicare in an accountable care relationship by 2030.1 Progress toward this goal continues its steady march, with almost 50% of Traditional Medicare lives now cared for by Accountable Care Organizations (ACOs), compared with less than 30% five years ago.2 Providers are increasingly adopting value-based care programs and models that allow them to practice medicine more holistically, while receiving substantial financial rewards.
The question for many primary care organizations is no longer whether to participate in value-based care, but which programs to consider and how to determine the best fit. Based on Pearl’s experience working with primary care providers across the country, we have consistently seen two CMS value-based payment models well-suited for primary care: the Medicare Shared Savings Program (MSSP) and the Accountable Care Organization Realizing Equity, Access, and Community Health (ACO REACH) model.
In 2024, as we expanded and diversified our network of primary care providers across the country, we also broadened our offerings across programs, models, and risk tracks to support the needs of providers and organizations at different stages in their journey toward value-based care.
In addition to supporting primary care organizations across a wider array of value-based payment models for Traditional Medicare, Pearl also continued our expansion into Medicare Advantage with new partnerships designed to enable primary care physicians to deliver more proactive, whole-patient care for a much greater proportion of the patients under their care.
#4 From Insights to Impact:
Navigating the Road from Volume to Value





In May and June, led by our CEO, a Pearl Health team drove from New York to Miami, with detours to visit primary care practices in 10 other major cities—including Philadelphia, Washington DC, Richmond, Raleigh, Nashville, Chattanooga, Atlanta, Savannah, Jacksonville, and Orlando—and a string of smaller metro areas and towns along a 2,000-mile stretch of American highway.
Along the way, we solicited responses to our Primary Care Pulse Survey, spoke with providers and clinical staff, and reported on some of the key challenges, impediments, and frustrations that primary care providers and organizations face today, as well as opportunities to achieve deeper satisfaction in their work, greater financial reward, and better outcomes for patients and the healthcare system.
While the Pearl team was on the road, we also conducted interviews from our roving recording studio with health system leaders, policy makers, academics, technologists, and advocates who are spearheading the healthcare system’s transition to value-based care.
We’re humbled and honored that so many of these healthcare leaders shared their insights with us, and we’re proud to elevate their voices as they ask hard questions, challenge outmoded assumptions, and share their ideas for how to deliver better outcomes for patients, providers, and the healthcare system at a lower cost.
Interested in learning more from leaders across the US healthcare system? Read Pearl Health’s Top 50 Value-Based Care Thinkers of 2024, which features quotes and insights from a broad cross-section of US healthcare and offers diverse perspectives on the challenges and opportunities presented by the transition from volume to value.
#5 New Faces, Bold Vision:
Growing & Evolving with Purpose
Over the past year, we’ve welcomed and elevated strategic leaders who bring invaluable experience, fresh perspectives, and a strong commitment to Pearl’s mission. They have joined Pearl’s leadership at a pivotal moment in our company’s evolution and are already making an impact in fostering a culture of collaboration, innovation, and excellence. We welcome these new leaders who are helping to shape the future of our organization and we’re excited for all we will accomplish together in 2025 and beyond.
Leadership Hires in 2024
Leadership Promotions in 2024
Pearl is led by experts in provider-enablement, risk-bearing, and technology, with a mission to help primary care organizations deliver proactive, efficient, patient-centric care. Our team is the heart of everything we do. United by a shared mission, they bring dedication, intelligence, and passion to solving some of the most complex and intractable problems in healthcare. They are the reason for our success, and we couldn’t be prouder of this dynamic and inspiring group.
We’re expanding in several functions, including engineering, sales, marketing, operations, and customer success. Interested in joining our team in 2025? Check out opportunities on our Careers Page.
Centers for Medicare & Medicaid Services, “CMS Announces Increase in 2023 in Organizations and Beneficiaries Benefiting from Coordinated Care in Accountable Care,” January 17, 2023.
Centers for Medicare & Medicaid Services, “Participation Continues to Grow in CMS’ Accountable Care Organization Initiatives in 2024,” January 2024.
Centers for Medicare & Medicaid Services, “CMS Finalizes “Pathways to Success,” an Overhaul of Medicare’s National ACO Program,” December 2018.