Pre-visit planning is essential for primary care practices to proactively manage their patient panels. If approached with straightforward processes and supporting technology, the process can lend efficiency to downstream encounters, delegate administrative tasks to less time-sensitive settings, and significantly decrease administrative burdens on care teams.
We encourage practices to incorporate elements of pre-visit planning into their encounter close workflows to streamline process, establish best practices that are easy to follow, and ensure consistency over time.
Ideally, pre-visit planning consists of several broad domains, including:
- Chart review to discover new events, diagnoses, and results; this is particularly important for pathology that has occurred outside of the PCP’s office.
- Longitudinal consideration of chronic health conditions, as well as their maintenance, trajectory, and control (e.g. diabetes management metrics) with capture and recapture of Hierarchical Category Condition Codes (HCCs), as these directly determine the patient’s overall risk benchmark.
- Consideration of intersecting social or medical needs, including Advanced Care Planning (ACP) and Social Determinants of Health (SDoH).
In our experience, establishing a consistent routine for pre-visit planning helps practices to provide better, more proactive patient care, improves provider and patient experience, and enables greater success in value-based care arrangements, such as ACO REACH.
Pearl is here to help.
Practice staff can use Patient View within the Pearl Platform to prepare for Medicare appointments by scanning for important changes since a patient’s last visit, including: new medications that should be reconciled, diagnoses that should be re-evaluated, and recent activity that should be asked about.
Our technology platform distills clinical and administrative patient data across providers and facilities down to what’s essential for providers to stay up to date on patients over time, surfacing actionable insights at a glance.
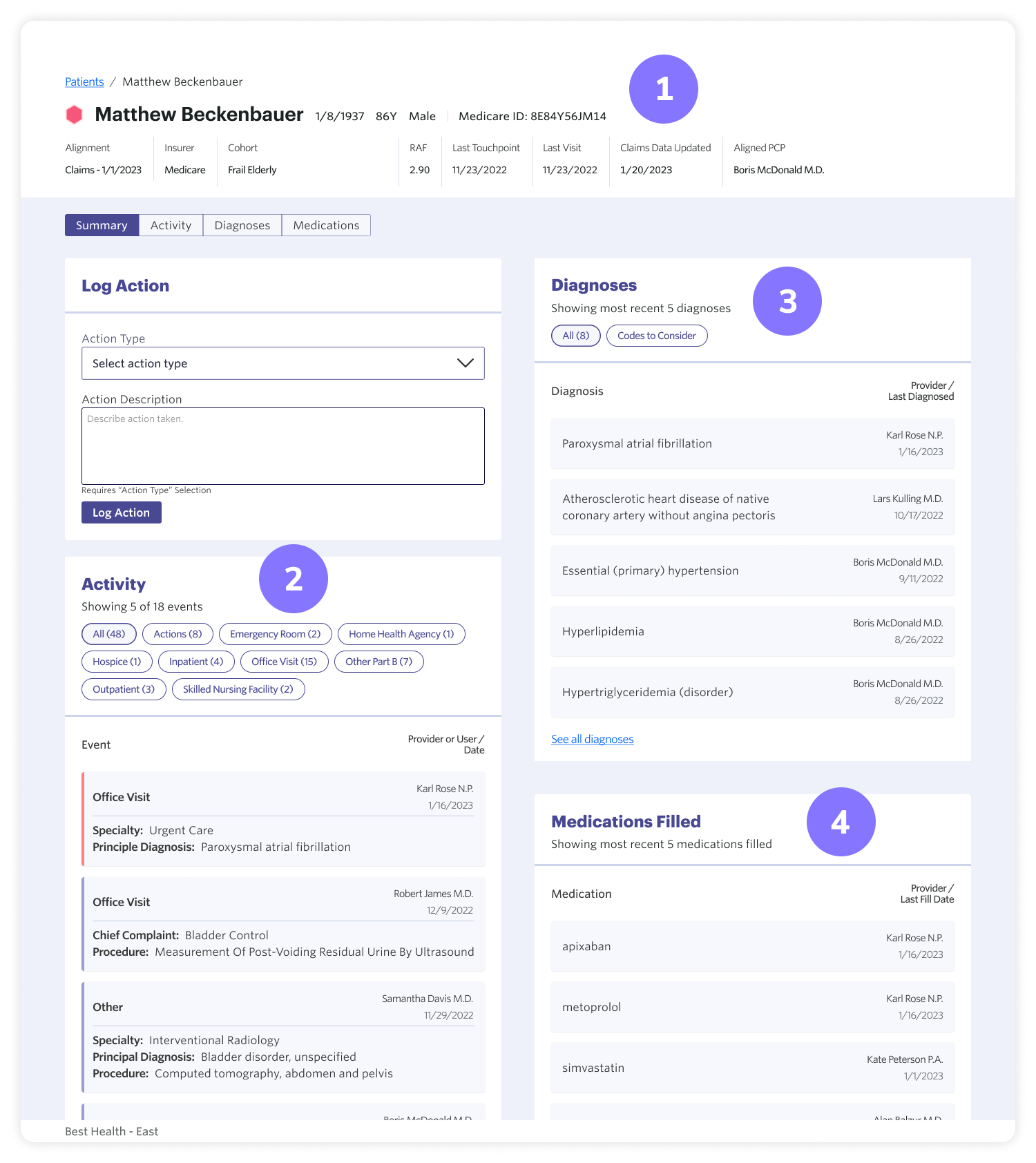
- Summary — provides an at-a-glance view of a patient’s age, frailty cohort, and activity status.
- Activity — shows recent hospital, emergency/urgency, and clinic visits, positioning providers to bolster care coordination and/or identify new intersecting health conditions or treatments (e.g. therapies, vaccines, interventions).
- Diagnoses — offers insight into conditions that may have emerged outside of the primary care office.
- Medications — identifies new, modified, or discontinued prescriptions, as well as prescriptions from other providers,enabling PCPs to maintain an accurate medication list, empowering high-reliability care.
In our experience, high-performing clinics often adopt common tactics for pre-visit planning, so we’d like to share some best practices:
- Develop an internal visit checklist, particularly for high-risk or high-acuity patients.
- Create check-ins or huddles, wherein the care team collaborates on patient needs.
- Delegate and handoff tasks to non-provider team members — much of this work can and should be performed by support staff.
- Click here to check out the AMA STEPS forward module on pre-visit planning for tips, tricks, and templates to help you get started.
We are proud to partner with PCPs across the country to build a healthcare system that is more sustainable, and we’re excited to continue developing technology and best practices to help our provider partners deliver more holistic, longitudinal patient care.