We are proud to announce that we have raised $75 million in our Series B funding round, led by Andreessen Horowitz’s Growth Fund and Viking Global Investors, with follow-on funding from AlleyCorp, SV Angel’s Growth Fund, and other leading investors. The round is comprised of $55 million in equity capital and an anticipated $20 million in a line of credit. This round brings Pearl’s total funding to date to more than $100M.
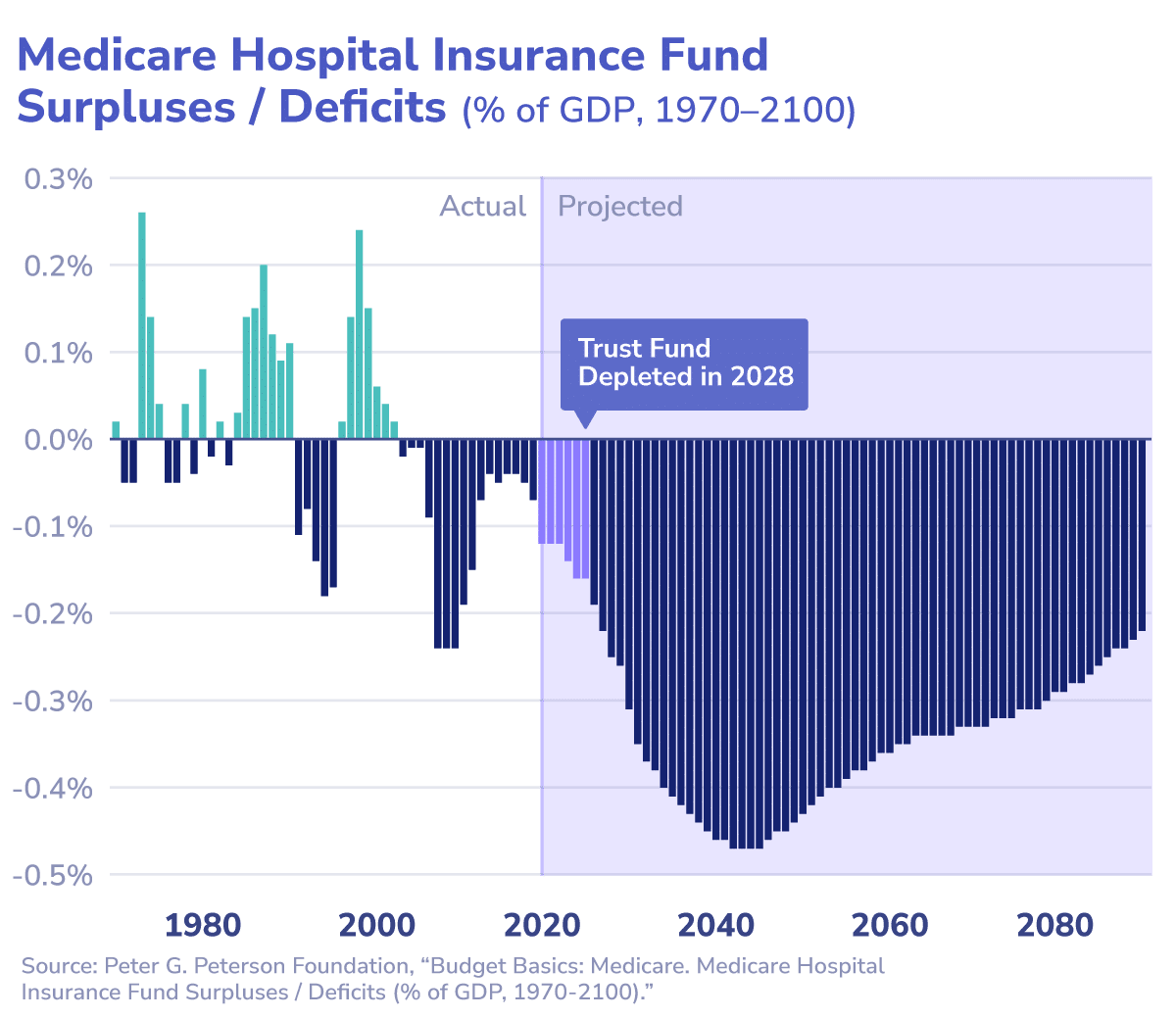
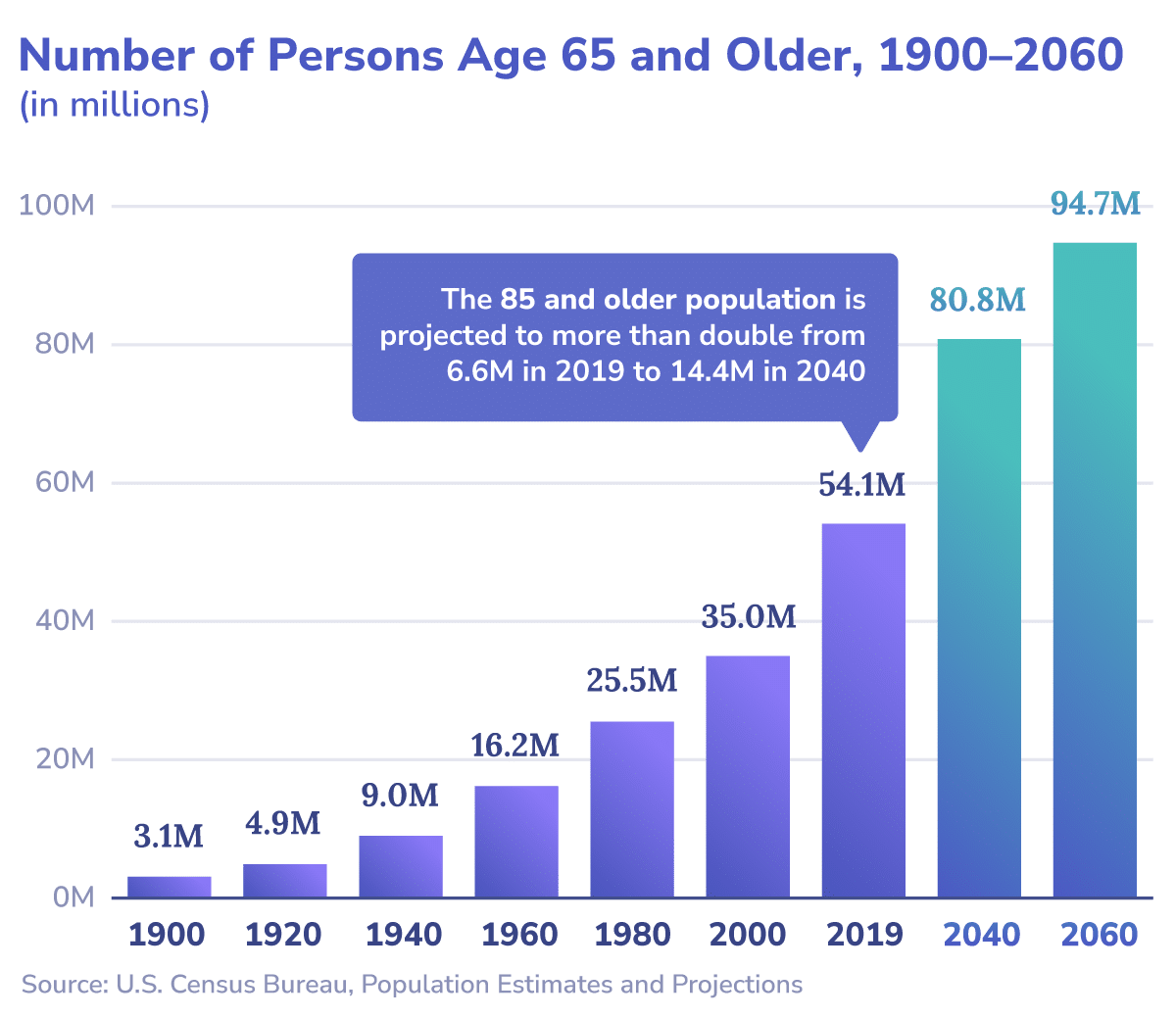
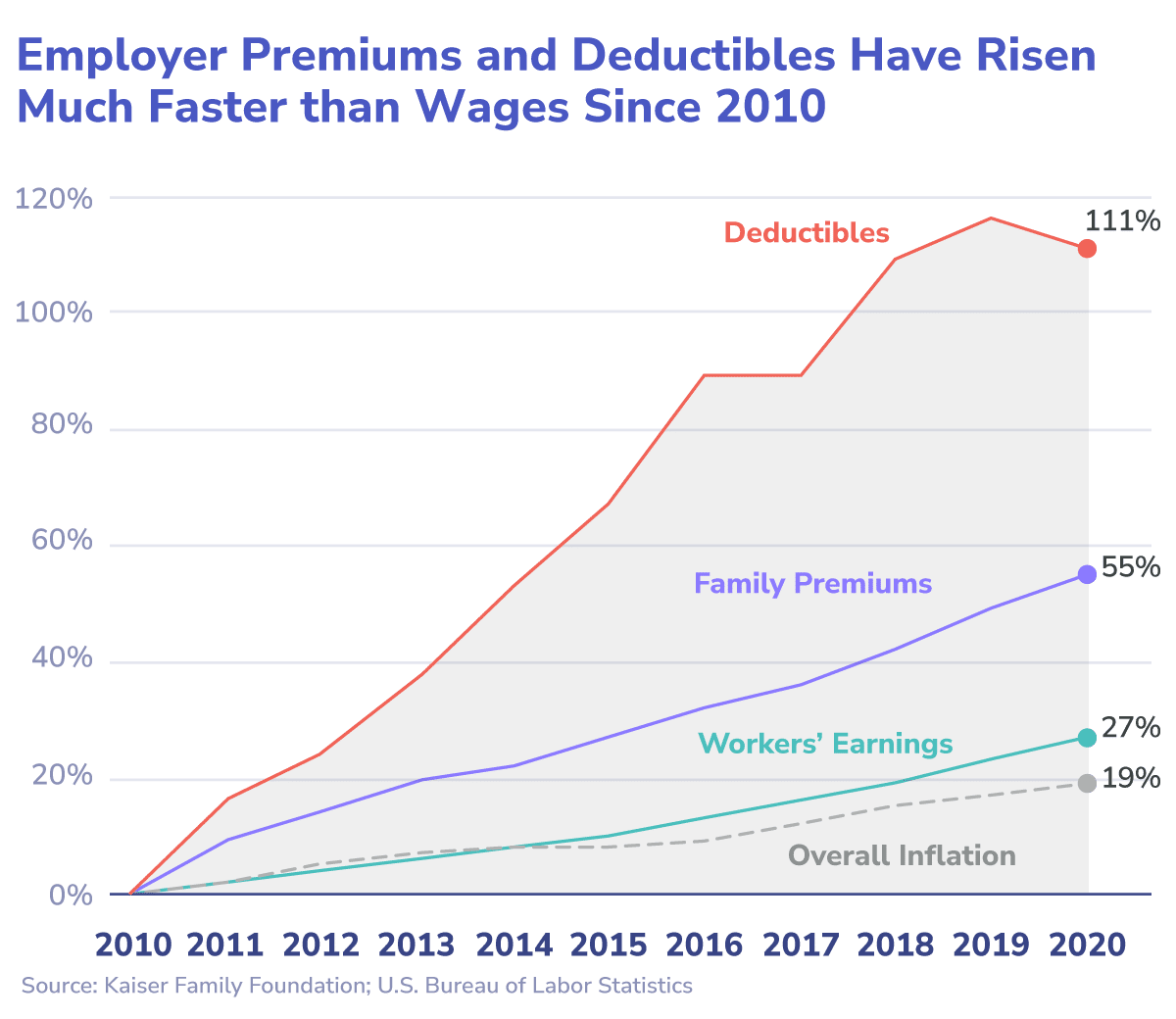
With the Medicare trust fund on the verge of bankruptcy,1 an aging population,2 and healthcare costs steadily increasing,3 the US healthcare system is approaching a financial breaking point. Meanwhile, primary care is overburdened,4 undervalued,5 and inefficiently used,6 and chronic conditions are rising in prevalence and severity,7 resulting in poor health outcomes that are often avoidable and exacerbating existing strains on the system.
Increasing Risk Liquidity Through Strategic Growth
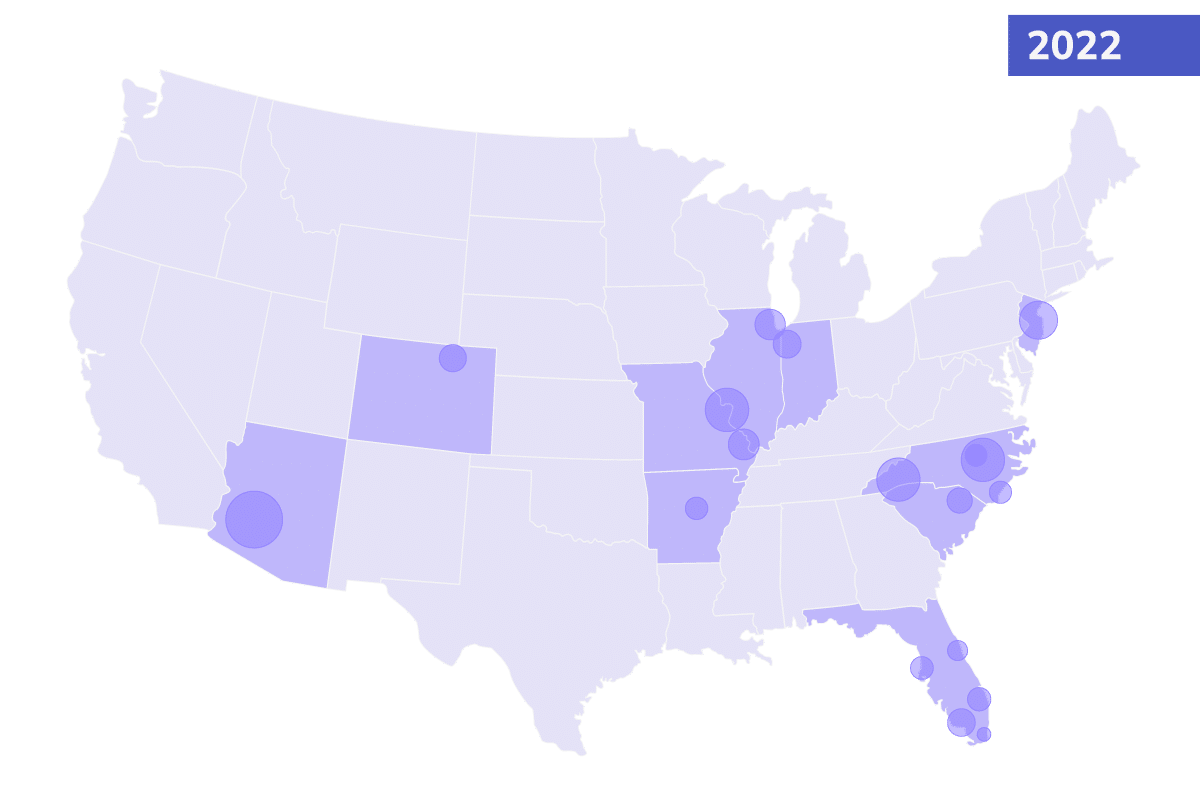
Over the past year, more than 800 primary care providers across the country partnered with Pearl to align payments with patient health and leverage emerging data and technology to achieve better outcomes more efficiently. We’re thrilled to welcome this new cohort of PCPs, who are committed to delivering value for their patients and for the healthcare system.
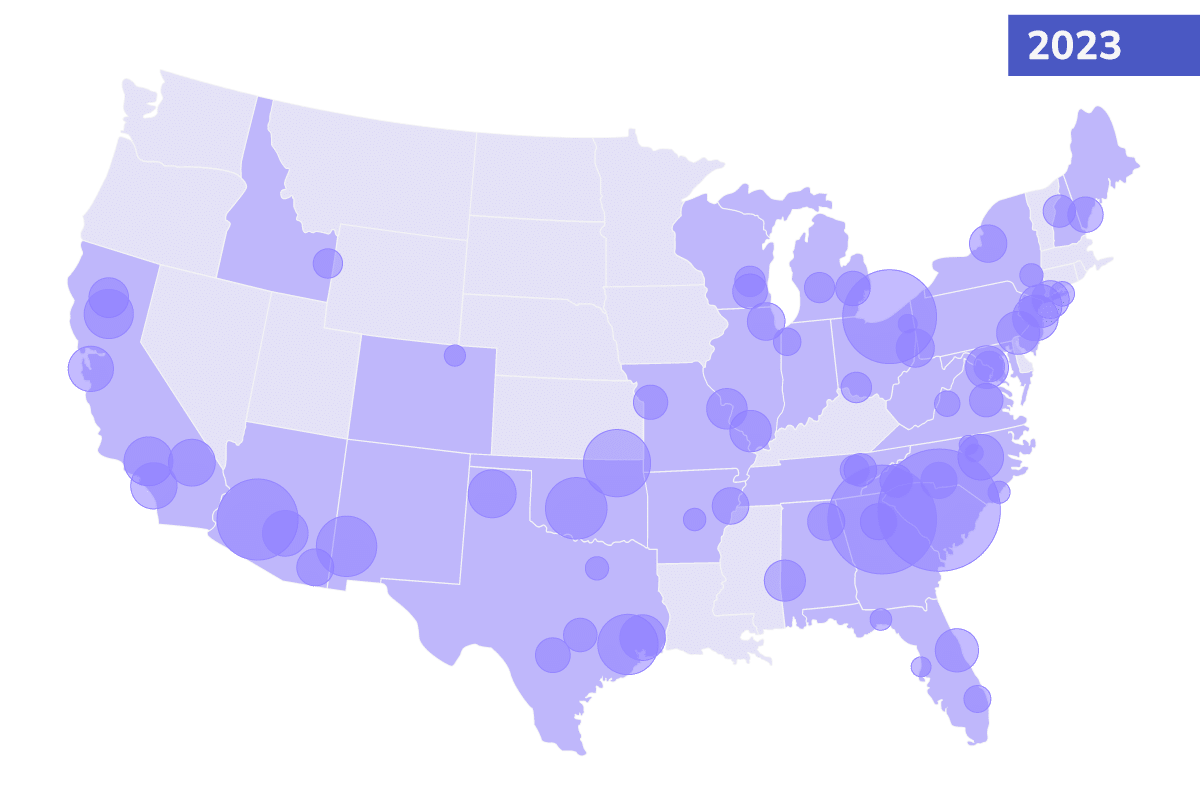
As we expand our network of enabled providers who can cooperate in risk-based arrangements, this will increasingly enable us to invite more payers to our model, who will, in turn, offer more risk-based models for our providers. This consolidation will empower providers increasingly to commit to this new healthcare system, and Pearl’s increased scope and insight will afford greater success to these partnerships.
While we started with traditional Medicare, we believe there is value in aligning the entirety of a practice’s panel to a better incentives structure. Our next stop will be working to expand our footprint to forward-thinking Medicare Advantage plans, so our provider partners can treat all seniors in a proactive, data-driven way. And be rewarded for it.
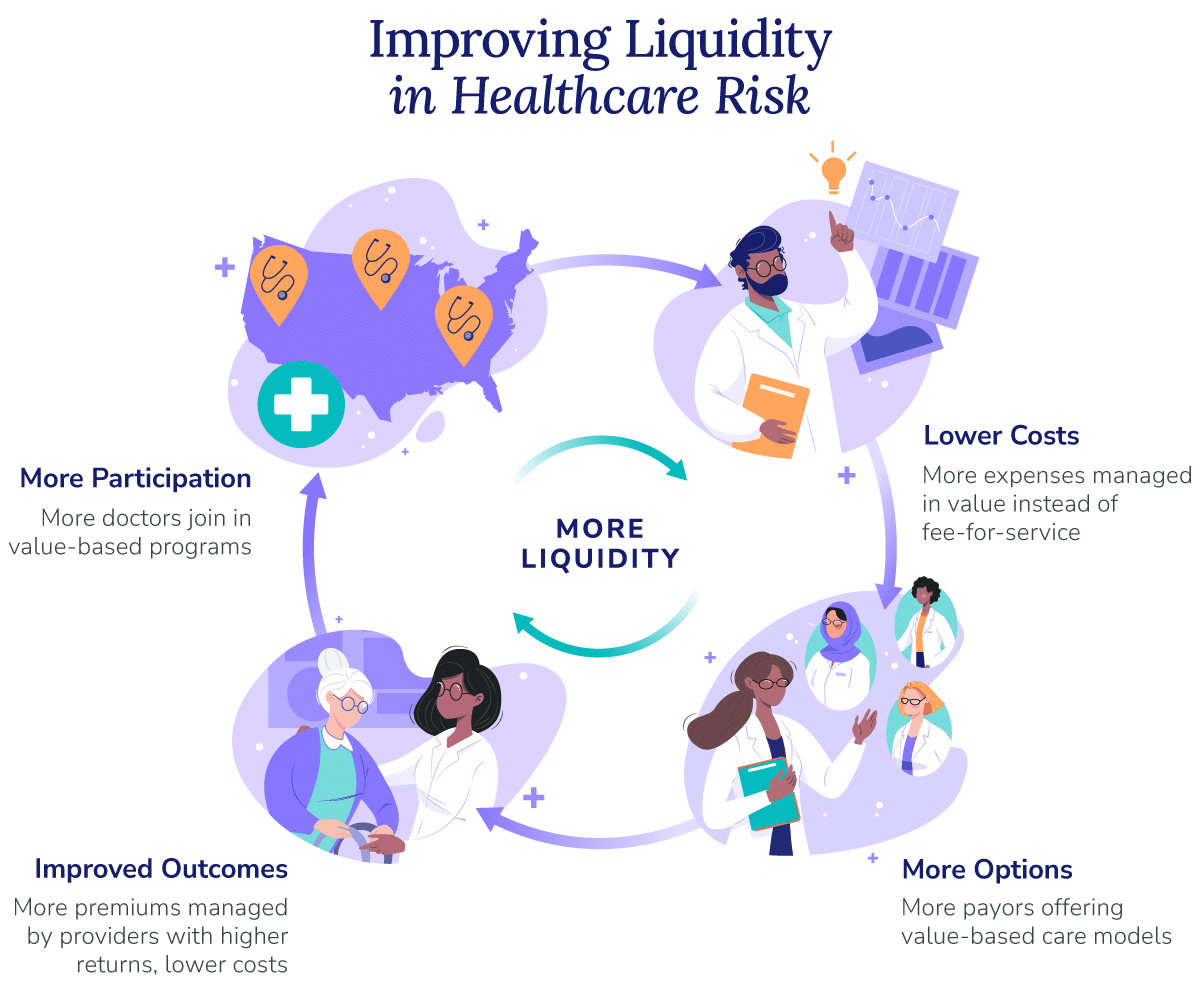
Our network growth creates a virtuous cycle: improving liquidity in the market for healthcare risk management, breathing oxygen into a financially broken system, and pushing toward efficiency and savings instead of volume and expenditures.
Generating Insights to Automate Value
In 2022, we launched the first version of the Pearl Platform: technology purpose-built to enable PCPs and clinical staff with insights that help them proactively manage Medicare patient panels with less work, deliver higher-quality care at a lower cost, and drive continuous improvement.
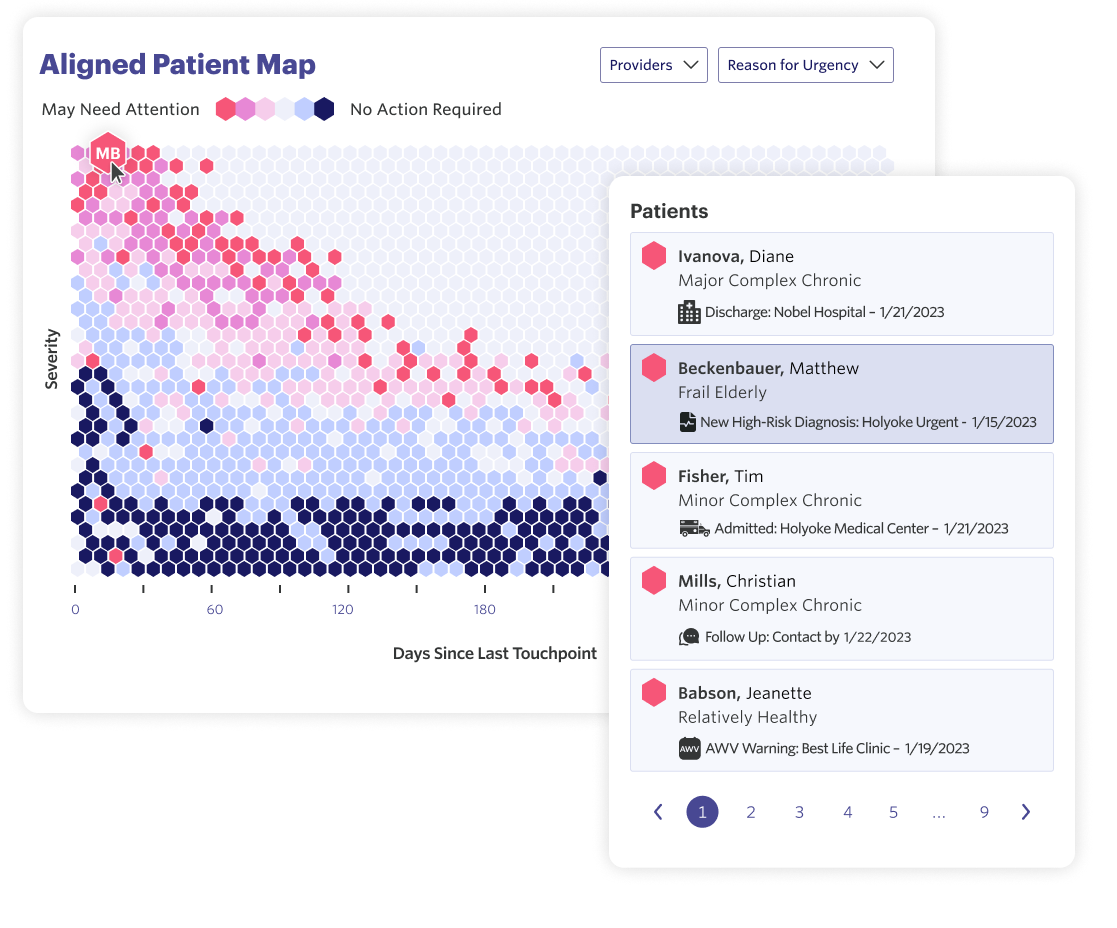
The platform is powered by data science models that distill complex information from across the entire healthcare system into what’s most important to enable proactive, whole patient care. We have taken a principled approach to developing and evolving the Pearl Platform, prioritizing ease-of-use, minimizing the administrative load required from users, and surfacing simple, actionable insights.
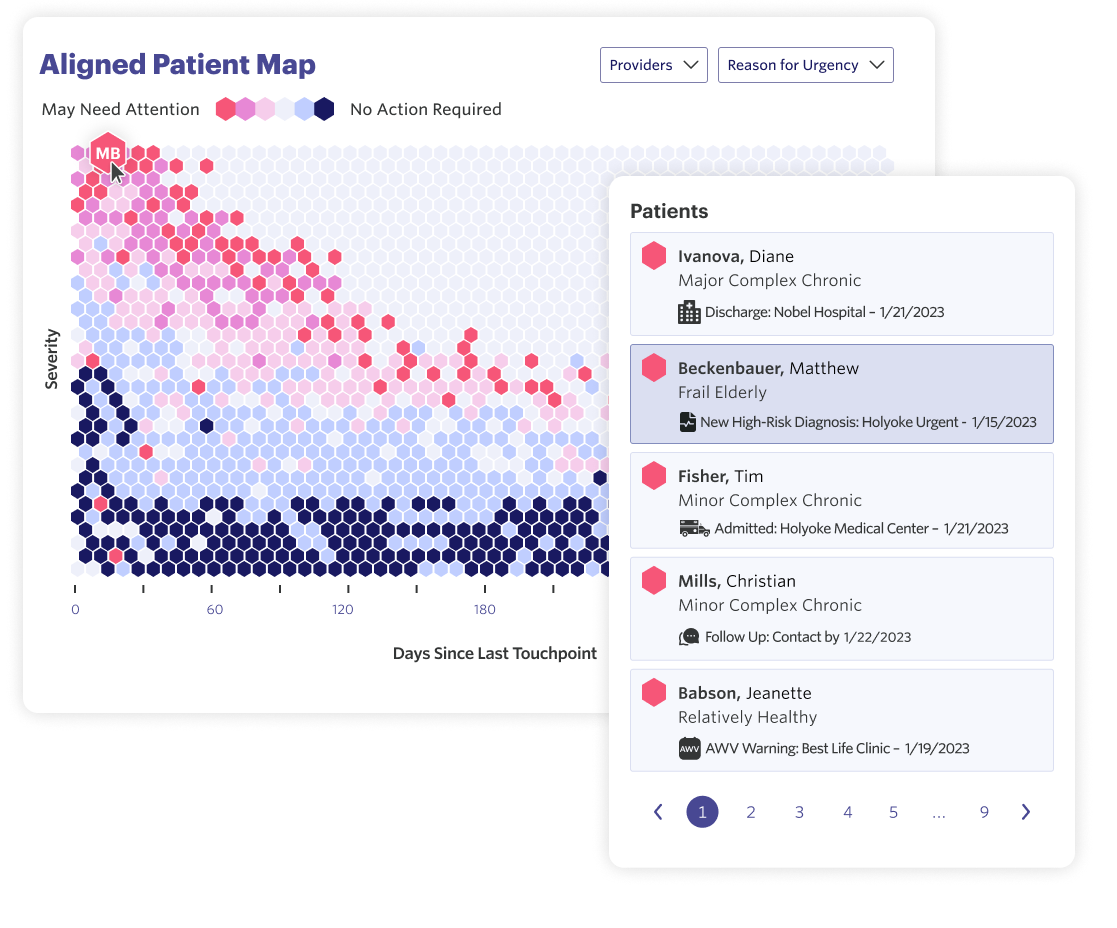
Through the Pearl Platform, providers and clinical staff can more easily understand their performance and identify the patients most likely to need attention across a patient panel. They can also explore detailed patient-level information with data across providers and facilities (e.g. hospital admissions, new diagnoses, new medications) to get a holistic, longitudinal view across a patient’s care journey.
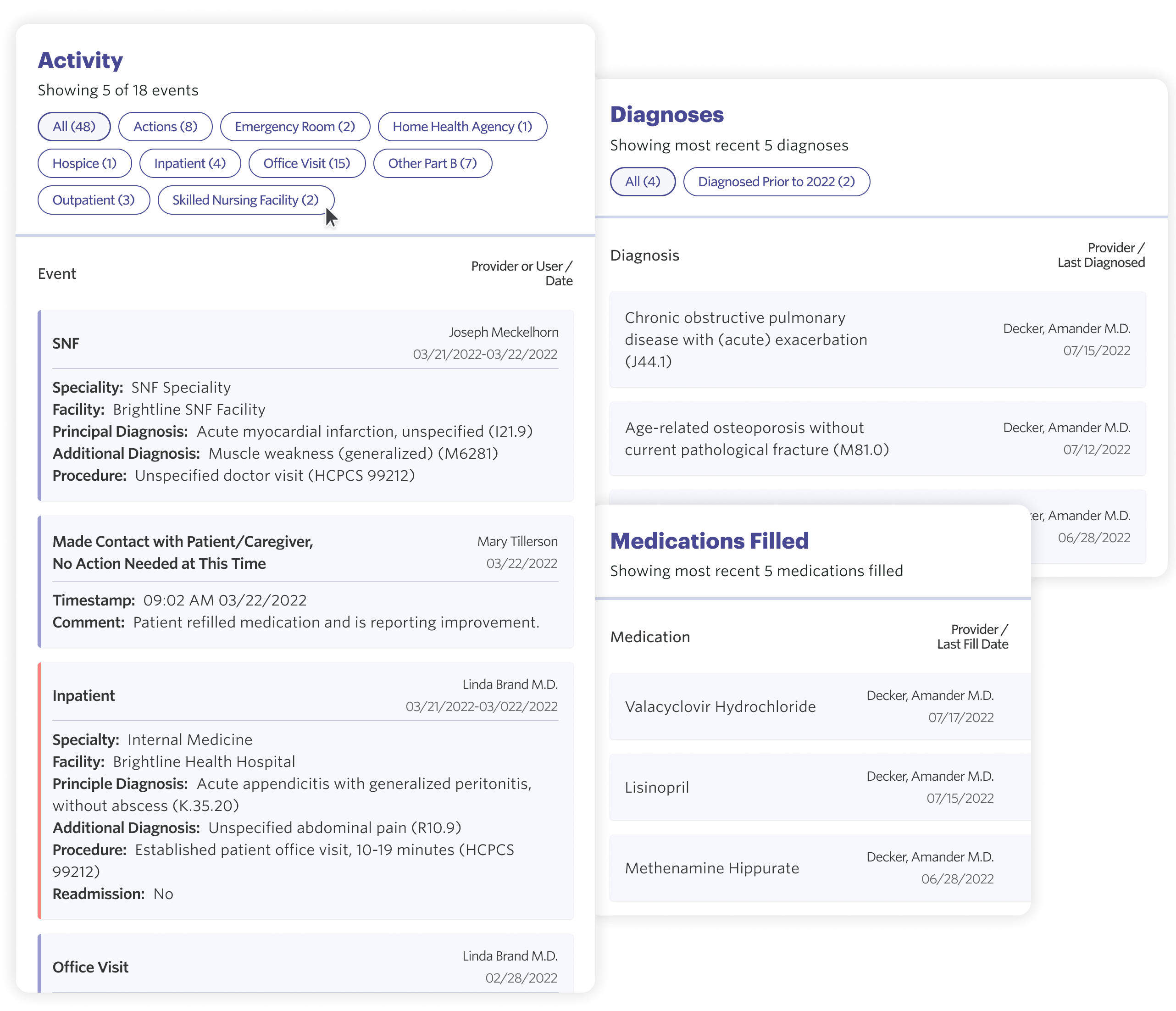
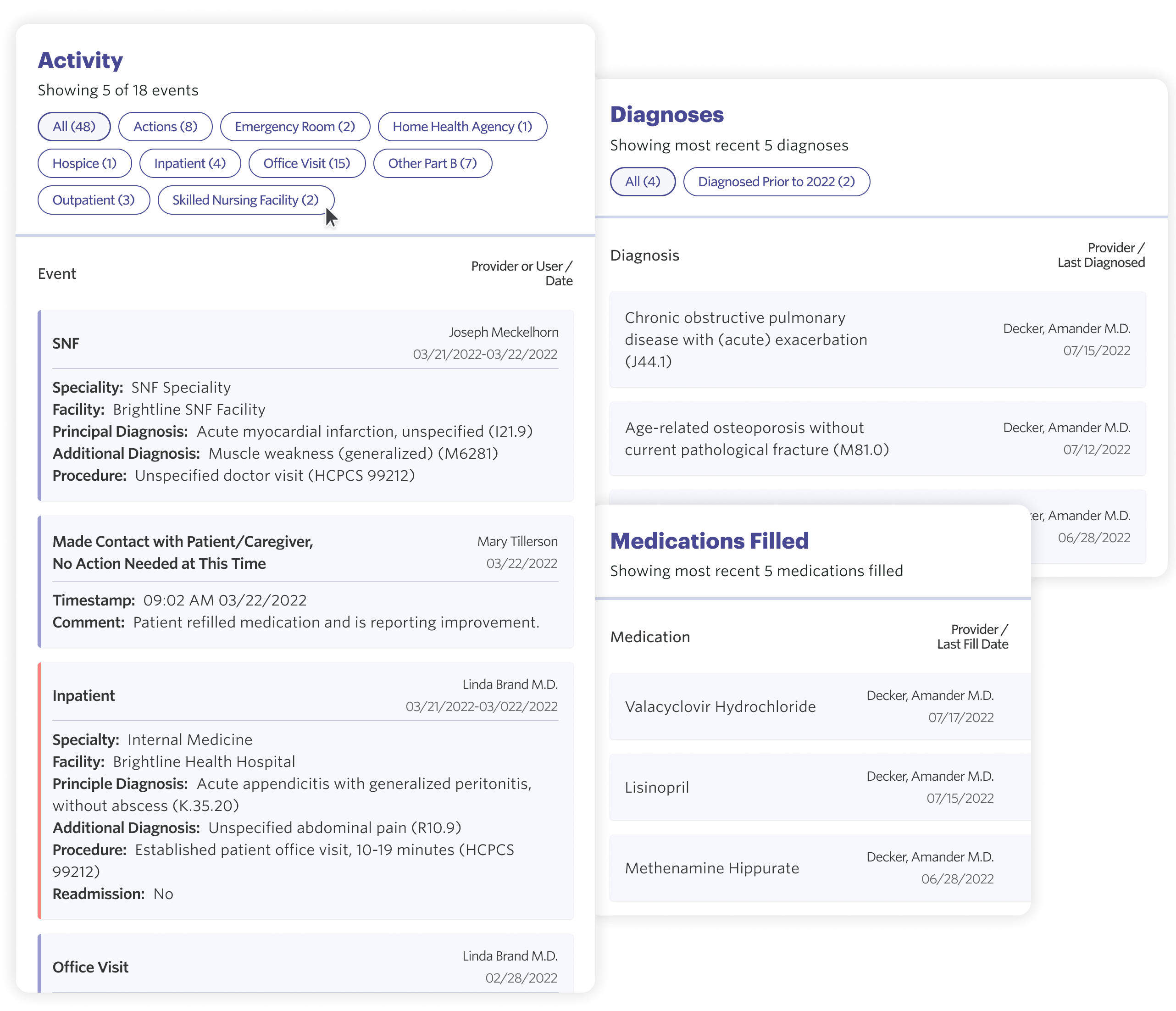
We believe the best way to empower providers to manage healthcare risk is to ensure they have unparalleled visibility into their patients’ healthcare utilization and needs. The Pearl Platform equips providers and clinical staff with timely admit, discharge, and transfer (ADT) alerts, so they have the information they need to effectively coordinate care following acute or post-acute events and prevent costly, avoidable hospital readmissions.
Finally, turnkey reporting gives primary care organizations strategic visibility into the most important determinants of success in value-based models and helps identify where they could deliver better care at a lower cost — without hours spent in spreadsheets, checklists, or reports on quality measures.
Creating a Marketplace for Efficient Risk Management
We believe that physician enablement technology with a focus on primary care is critical to improve outcomes across patient panels and lower costs across our healthcare system; however, PCPs will of course continue to require support from specialists for those patient cases beyond the purview of general medicine.
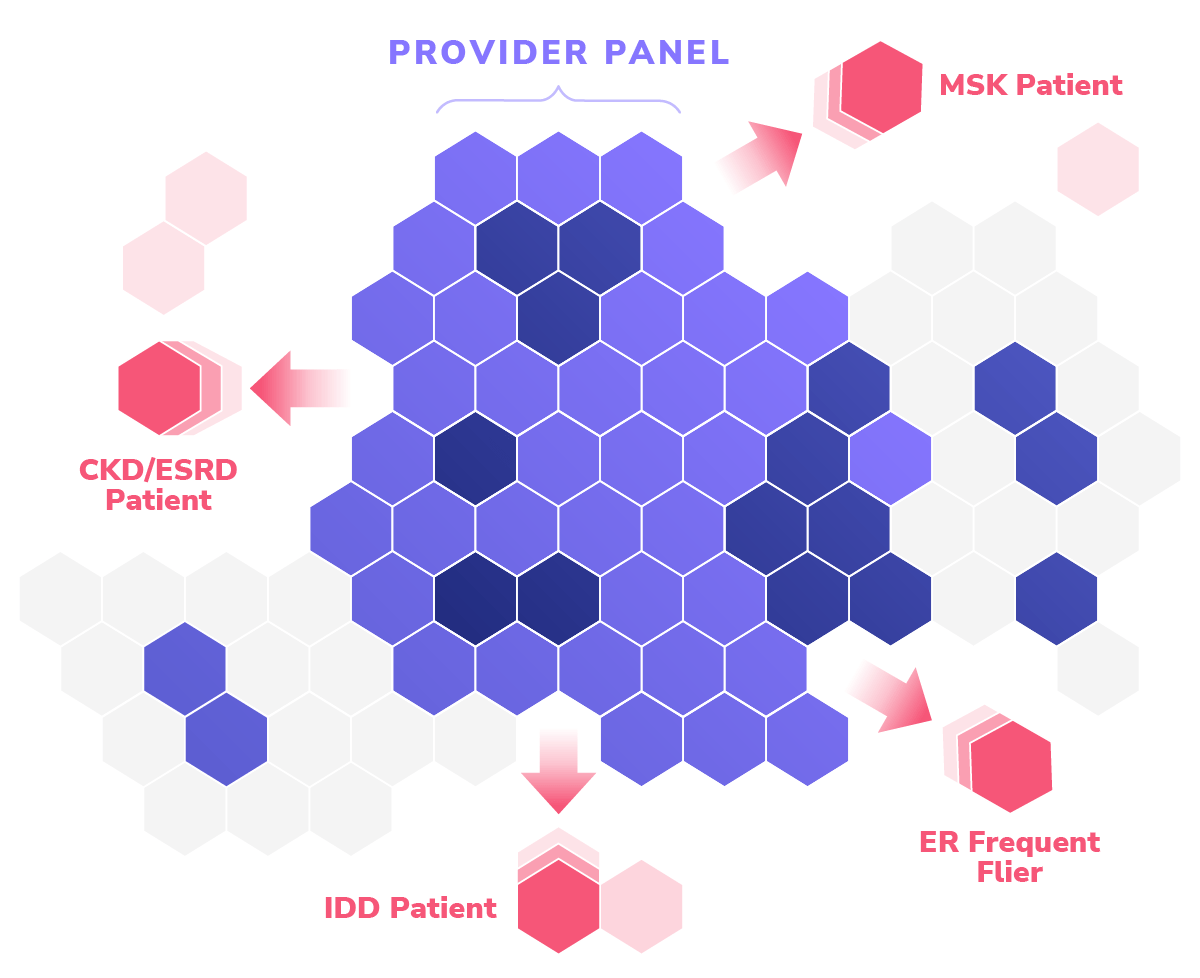
In recent years we have seen a proliferation of mission-driven companies founded to manage distinct cohorts of patients based on the clinical disease burdens they exhibit, bringing to bear novel care models and eschewing traditional healthcare network constructs. Pearl sees this new landscape of Specialty Risk Partners as an opportunity to obviate the problems presented by most local market dynamics and move toward better aligned virtual care teams supported by targeted local assets.
We have already laid the groundwork with early Specialty Risk Partners that have demonstrated high-quality, efficient outcomes via appropriate care models for populations most prevalent amongst our provider partners’ panels. As time goes on, we will continue to develop integrated tooling to better manage at-risk populations, while aligning these partners with PCPs through both the Pearl Platform and financial incentives.
Building Our Team and Values-Based Culture
At Pearl, we have always believed that our team — and, above all, our culture — will be the ultimate reason for our success or failure. We have created and will continue to iterate on company values that serve as our north star through difficult decisions and growth.
As we enter the next phase of our evolution as a company, we’re confident that we are building the right team and culture to meet the moment.
Our Board of Directors
Vineeta Agarwala, MD
Board Member
a16z
Jeffrey De Flavio, MD
Executive Chairman
ALLEYCORP | Groups
Michael Kopko
Board Member, CEO
OSCAR | BRIDGEWATER
Scott Kupor
Board Member
A16Z
Kevin Ryan
Board Member
ALLEYCORP
Our Management Team
Gabriel Drapos
Chief Operating Officer
Centivo | Oscar
Jennifer Rabiner
Chief Product Officer
Hint Health | Athenahealth
Matt Solnit
Chief Technology Officer
Akamai
Joseph Cianflone
Executive Vice President, Finance and Strategy
PSP Investments | Black Diamond Asset Management
Steven Duque
Chief Growth Officer
Catalant | Happie
Jon Goldin
Chief Legal Officer
Wachtell Lipton | Teneo
Our team of provider-enablement, risk-bearing, and technology experts are thoughtfully building a values-based team to democratize access to healthcare risk, align incentives with patient outcomes to deliver higher-quality care at a lower cost, and to make our healthcare system more sustainable.
Interested in learning more? We are hiring across functions, including engineering, product, sales, marketing, customer success, and finance. Check out opportunities on our Careers Page.
- Peter G. Peterson Foundation, “Budget Basics: Medicare. Medicare Hospital Insurance Fund Surpluses / Deficits (% of GDP, 1970-2100).”
- U.S. Census Bureau, Population Estimates and Projections. Cited in U.S. Department of Health and Human Services, Administration of Community Living, “2020 Profile of Older Americans,” May 2021.
- Statista, “U.S. Health Expenditure as Percent of GDP from 1960 to 2021.”
- University of Chicago, “Primary care doctors would need more than 24 hours in a day to provide recommended care,” August 2022.
- PCPs are under-compensated, compared both to other verticals of the healthcare system (among the lowest ranked specialties by annual compensation) and to the value they bring to that system (the average PCP generally earns $266k, but influences ~$10M in downstream healthcare costs). Sources: Farzad Mostashari, Darshak Sanghavi, Mark McClellan, “Health Reform and Physician-Led Accountable Care: The Paradox of Primary Care Physician Leadership,” JAMA, May 2014. Medical Group Management Association (MGMA), “New MGMA research finds physician compensation on the rise,” Cision PR Newswire, May 2019.
- Healthcare spending per capita in the US is about twice that of comparable countries; yet, US healthcare consumers engage in routine care less often. Higher (and more efficient) utilization of primary care services can decrease systemic costs overall by mitigating risks before chronic conditions develop or acute events occur. Sources: Peterson-KFF Health System Tracker, “Health consumption expenditures per capita, U.S. dollars, PPP adjusted, 2020 or nearest year.” OECD Health Statistics, “Number of doctor consultations per person (2017 or most recent available),” 2019.
- Wullianallur Raghupathi and Viju Raghupathi, “An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach to Public Health,” 2018.