We’ve been lucky to meet and speak with some of the great minds in healthcare as we built Pearl Health and through our time scaling Oscar, Clover, athenahealth, and many other places. The US Healthcare system is expensive due to a variety of factors, including high unit costs and the complexity of our system, as well as an under-investment in primary care services and wellness. 
The Top 6 Sources of Waste in Healthcare and ways to solve it!
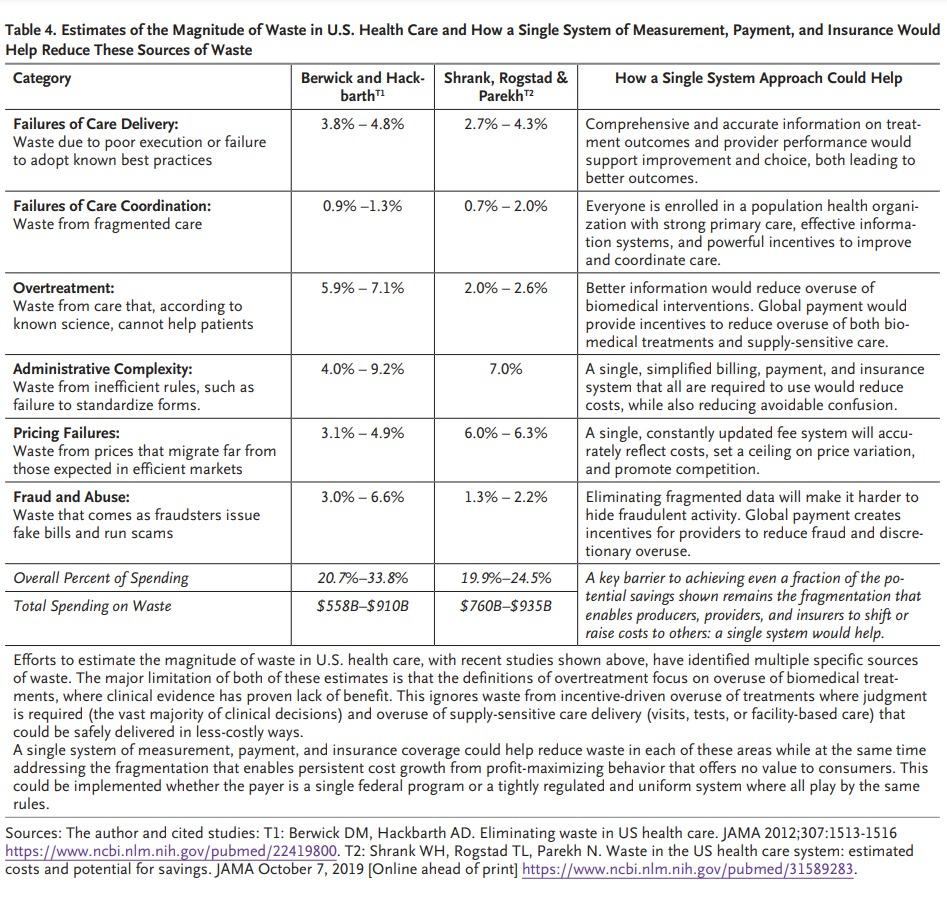
- Administrative Complexity – the lack of simple technology and standard platforms that enable payments, billing, and the provision of services in a competitive and cost effective way. Examples include complex billing and prior authorization requirements, as well as non-standard practice management systems that do not interoperate well with other environments. Answer: technology and standards should push toward simplicity and interoperability.
- Over-treatment – the unnecessary provision of care. Examples include excessive prescriptions, MRIs, and unnecessary bed stays or healthcare overconsumption. Answer: changing our compensation model to budget- or benchmark-based management vs. expense generation.
- Fraud and Abuse – fake or exaggerated healthcare bills or billing practices and outright violation of laws and payment contracts. Examples include billing government programs for services never rendered, upcoding services that were not actually provided or justified, and outright theft through reimbursement cheating. Answer: changing our compensation model to budget- or benchmark-based management vs. expense generation.
- Pricing failures – the fact that no one knows what they are buying, what it costs, and how much they have to pay for it leads to a market failure for those who receive healthcare services as well as those who request or prescribe it. Answer: pricing transparency, global budgeting, and movement toward first party payments.
- Care Delivery and Supply Chain Failures – the missed delivery of proper care when required or the provision of services when needed leading to unnecessary escalations of condition acuity or compounded expenses. Examples include lack of physician access leading to emergency room visits, missed prescriptions precipitating condition deterioration, and general absence of wellness and other investments to remediate conditions before they become severe. Answer: physician-centered delivery systems with improved payment models to reward and compensate preventative and interventionary care.
- Care Coordination – the missed value of patients being managed and monitored by primary care doctors or population health programs so they can have their needs met as they occur. Answer: physician-centered delivery systems with improved payment models to reward and compensate preventative and interventionary care.
Addressing this waste can help pull +$500B out of the cost of our healthcare system with no quality tradeoffs. By investing in innovation and attacking waste in healthcare, we at Pearl are helping to improve the sustainability of our healthcare system and redeploy resources to where they can get a higher return for the health of our country.